Tuberculosis still kills over 1.2 million people a year. In a two-part essay by Kamal Nahas for Asimov Press, we explore why and how to change that.
In the 1924 novel, The Magic Mountain, Thomas Mann describes a sanatorium patient named Anton Ferge as he undergoes a painful tuberculosis (TB) treatment. “I lie there with my face covered, so I can’t see anything,” Anton says. “I feel myself being pinched and squeezed, that is the flesh they are laying back and pegging down.”
Ferge’s harrowing treatment is a lung-flattening artificial pneumothorax, an outmoded practice involving the injection of nitrogen gas into the chest cavity to compress a TB-ridden lung. The goal of the procedure is to crush cavities hollowed out by the bacteria. And although Mann includes some literary flourishes, he accurately captures the crudeness of the procedure: “Then he begins, with a blunt instrument — it must be blunt, not to pierce through too soon…”
A TB patient is subjected to a pneumothorax operation.
Physicians working in the early 20th century had little choice but to treat the world’s most rampant infectious disease with methods such as these. Even after microbiologists discovered the bacterium that causes the illness in 1882, it wasn’t until the 1920s that researchers were able to develop a vaccine for TB.
These breakthroughs have significantly curbed cases, with vaccination reducing the odds of death by 74 percent. But even now, more than a century later, TB remains the deadliest infectious disease on Earth, killing about 1.2 million people every year.
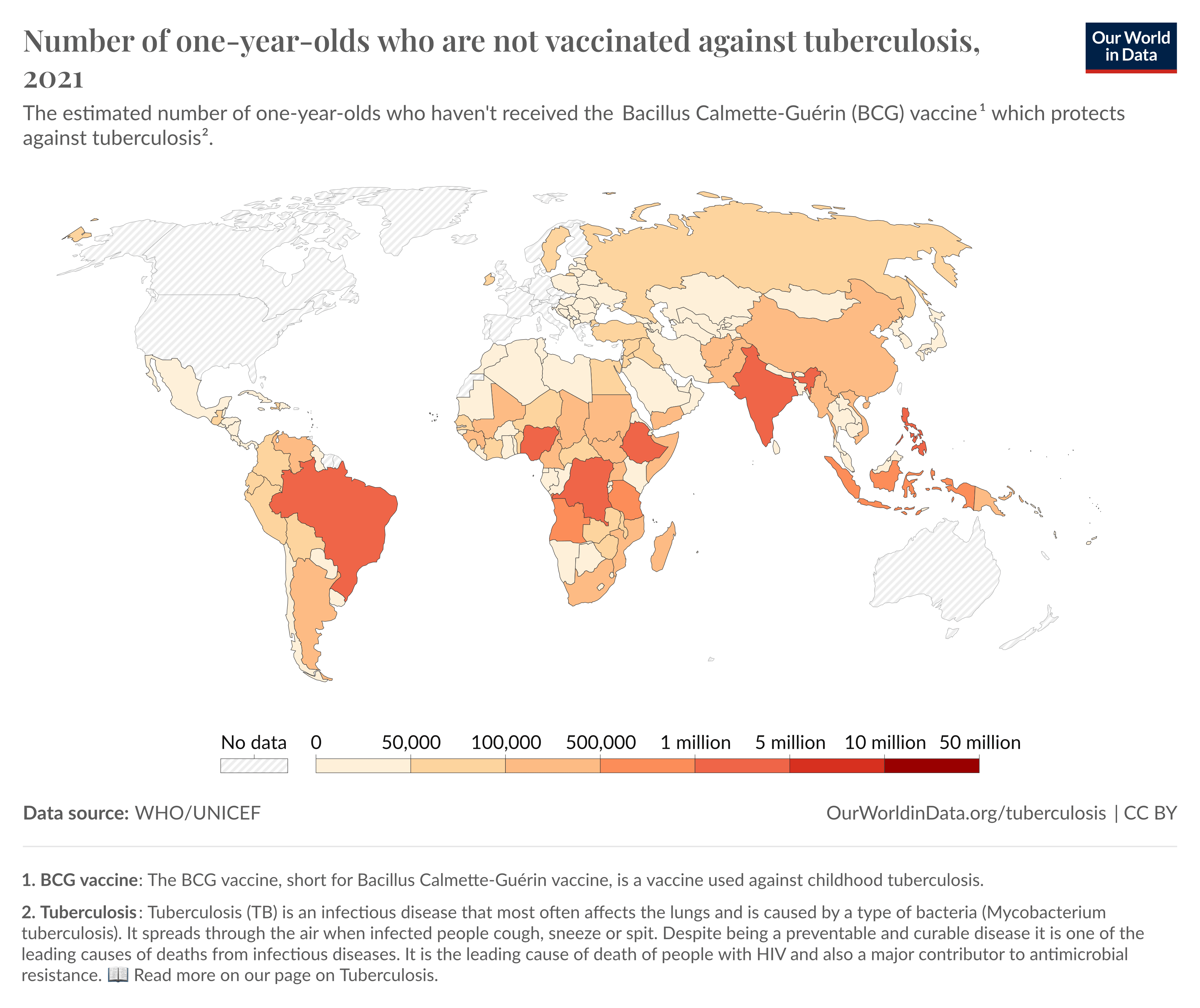
Despite TB’s prevalence, researchers have not produced and launched preventatives and treatments for the disease beyond a vaccine for children, developed in 1919, and antibiotic regimes similar to those developed in the 1950s. But they will need to do so if they want to meet the goals set out by the End TB Strategy, namely, to reduce TB cases by 80 percent and curb deaths by 90 percent before 2030.
As an undergraduate biology student, I spent some time in a TB lab working on antibiotic resistance — a growing concern for drug developers. The experience showed me that new therapies are needed not only to meet the targets laid out by the End TB Strategy but also to prevent drug resistance from negating the effectiveness of current therapeutics. Fortunately, some novel preventatives and therapies are in the works, including a vaccine equipped with adjuvants that efficiently prime the immune system and newer antibiotics against which the bacteria have yet to evolve resistance.
Still, while these developments provide cause for hope, each drug or vaccine faces a variety of challenges, ranging from financial incentives for clinical trials to the difficulty of discovering new antimicrobials that pass safety and efficacy tests.
Subscribe to receive essays from Asimov Press.
Always free. No ads. Richly storied.
Making a Vaccine with Ox Bile and Potato Essence
Two French bacteriologists named Albert Calmette and Camille Guérin set out to develop a vaccine against Mycobacterium tuberculosis at the beginning of the 20th century. Working at the famed Pasteur Institute, the duo began by figuring out how best to culture mycobacteria — a seemingly simple, but essential first step, given how no one at the time had yet come up with an effective way of growing these bacteria in the laboratory.
In a series of experiments performed between 1900 and 1908, Calmette and Guérin developed a recipe for a growth medium suitable for mycobacteria. To feed bacterial growth, they used potato extracts rich in sugar and other nutrients. In time, the bacterial populations would consume all the resources in the medium, so Calmette and Guérin had to periodically transfer a small number of bacteria onto fresh media — a process known as subculturing.
During the First World War, the French duo also invented a method to freeze their cultures in case wartime rationing limited potato supplies.1 However, ice crystals expand and shatter bacterial membranes, killing the microbes. To protect against this, Calmette and Guérin added a small amount of glycerin, a cryoprotectant, to slow ice crystal formation. Their mycobacteria cultures grew well in the amalgam and could be frozen and thawed time and time again. Finally, the team added ox bile, rich in fat-dissolving enzymes and bile salts, to disperse clumps of bacteria.
Camille Guérin (left) and Albert Camette (right) at the Pasteur Institute.
With their newly-optimized medium in-hand, the French scientists grew and repeatedly subcultured the bacterial colonies. They used M. bovis, a bacterial species related to M. tuberculosis, to develop the vaccine. This species is more adapted to infecting cattle than humans, so they reasoned it would be less likely to cause serious infections in people and be easier to work with during subculturing experiments.
Serendipitously, it was the subculturing step that became the key to developing a vaccine: As the bacteria adapted to the media over many growth cycles, they lost their ability to cause disease, becoming harmless microbes that could prime the immune system.
After 230 rounds of subculturing between 1908 and 1919, Calmette and Guérin produced a “live-attenuated” strain of the bacterium, unable to cause TB in cattle, guinea pigs, horses, or rabbits. Among other mutations, the subcultured M. bovisstrain lost three chunks of its genome, each several thousand base pairs long. The live-attenuated strain was renamed as the Bacille Calmette-Guérin (BCG) vaccine (“bacille” is French for “bacillus”, meaning rod-shaped bacterium).
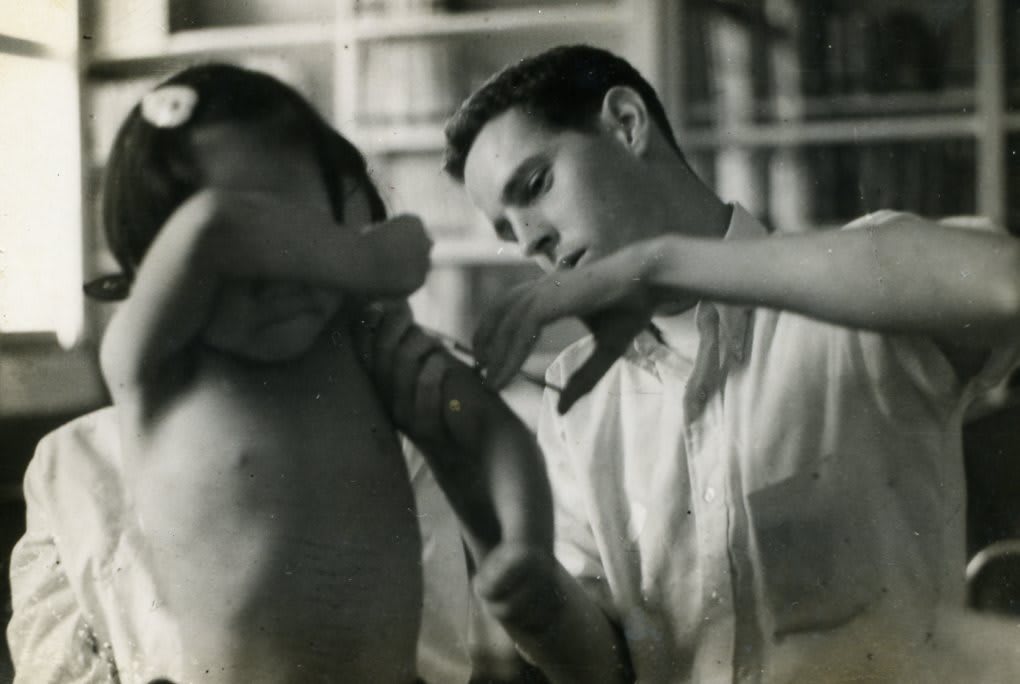
Based on early successes in animal experiments, doctors tested the vaccine on an infant whose mother had died of TB shortly after giving birth. The infant experienced no adverse effects, thereby suggesting the vaccine was safe. Physicians began to administer the vaccine to more and more infants, and in the following decade, over 100,000 vaccinated children reported no serious complications. Over 7.8 billion people received this same vaccine between 1980 and 2023, making it the most widely administered vaccination on Earth.
A 1994 review of 14 prospective trials and 12 case-control studies revealed that the BCG vaccine reduced the risk of TB by 50 percent. The vaccine is especially effective in children, protecting 60 to 80 percent from developing active TB. However, the vaccine provides less protection when given to adults. Chilean research participants aged 15 to 35 who received the vaccine during a case-control study, for example, only showed a 10 percent reduced risk of pulmonary TB. Adults fare less well because the vaccine’s effectiveness wanes over time: The memory T cells that confer long-lasting immunity die off after a few months, and older children have fewer of these memory T cells than younger infants.
Although dozens of studies suggest the BCG vaccine works, the same studies also show wide distributions in its efficacy. Some studies boast 80 percent efficacy while others suggest it is zero. The BCG vaccine is not as effective as, say, the live-attenuated cholera vaccine developed in 2016, which consistently protects against diarrheal disease 90 percent of the time within 10 days of vaccination.
One possible explanation for this variability stems from how the BCG vaccine is made. Researchers haven’t cloned and saved the initial BCG strain developed by Calmette and Guérin in the early 20th century. Instead, different vaccine manufacturers in Bulgaria, Denmark, Japan, Russia, and other countries have individually subcultured the BCG strain. Consequently, their strains may have accumulated genetic discrepancies, diverging over time from the original variant. These genetic differences are so pronounced that some strains have even relinquished a sizable fragment of the genome. Owing to these differences, it could very well be that some suppliers provide a more effective variant than others.
Another explanation is that harmless Mycobacterium species that are genetically related to M. tuberculosis are also in circulation, and people exposed to one of these strains tend to have reduced immunity against others. During vaccination, the BCG strain normally primes immune cells to destroy infections, and owing to its similarity to M. tuberculosis, the same immune cells cross-react with the pathogen. However, environmental bacteria complicate the picture. If present before vaccination, memory immune cells primed to destroy the environmental relatives might cross-react with and neutralize the BCG strain before it has a chance to set up an immune response against itself and M. tuberculosis.
A Peace Corps Volunteer administers the BCG vaccine to a six-year-old Korean boy. Credit: Neil Landreville
The vaccine certainly has pitfalls and does not protect everyone in every instance, but it is still used in nearly every country.2 And although the BCG vaccine doesn’t safeguard everyone who takes it, its widespread use leads to “herd immunity,” ultimately protecting those for whom the vaccine proved ineffective.
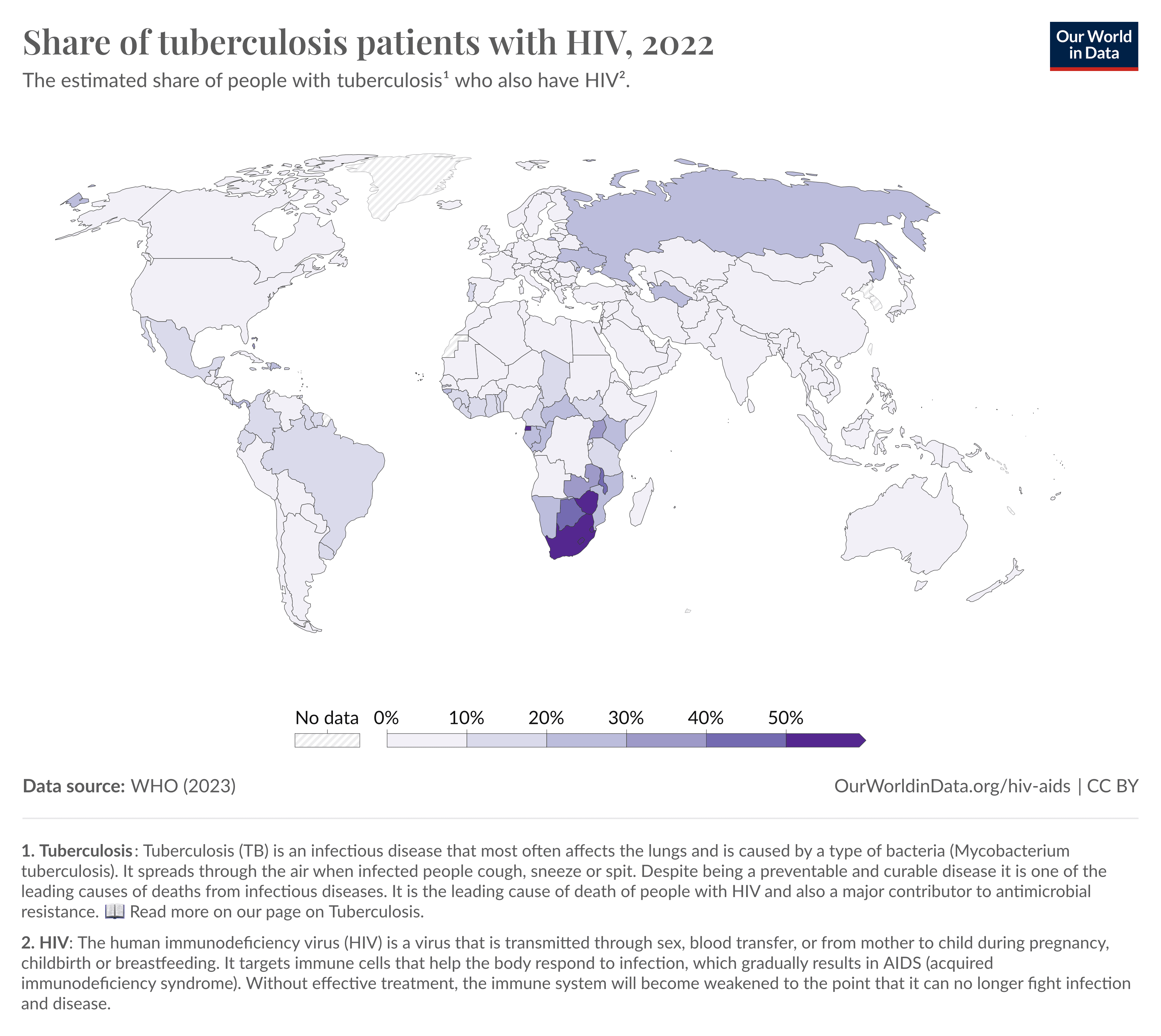
Herd immunity also shields those who cannot receive the vaccine in the first place. For the most part, BCG is safe and causes no serious complications; but because it contains a live-attenuated form of M. bovis, the WHO recommends against vaccinating those with underdeveloped immune systems, such as children infected with HIV, who may fail to mount an immune response capable of killing live pathogens.
People living in remote settlements without electricity, such as the Afar and Somali regions of Ethiopia, are also unable to receive the vaccine. The live-attenuated bacteria require refrigeration at 2–8°C, making it difficult to both transport and store for extended times.
Despite its safety and near-universal availability, the lackluster efficacy of the BCG vaccine hampers the End TB Strategy. We need better vaccines — and medicines — to quash TB.
Antibiotics From the Ground Up
Researchers unearthed the first TB drug from the ground.
Selman Waksman, an American soil microbiologist at Rutgers University, spent his early career studying how bacteria and fungi influence the chemistry of soils. One day, he and his team came across a soil bacterium that appeared to kill other bacterial species in its proximity.
With the help of eight other researchers, including a PhD student named Albert Schatz, Waksman spent five years isolating the bacterium in question, Streptomyces griseus, and harvesting its toxic chemical — the antibiotic streptomycin.3 Before testing whether this antibiotic could be used to treat TB in humans, Waksman shipped the antibiotic to veterinarians at the Mayo Clinic who specialized in TB animal research. However, Waksman’s lab did not possess the facilities required to produce large volumes of the chemical, so researchers at the clinic had to stretch the 10 grams of streptomycin between four guinea pigs over a three-month period.
The drug didn’t cure the animals at such low doses, but their health did improve, hinting at the drug’s efficacy. Based on these results, Waksman asked the pharmaceutical company Merck to mass-produce streptomycin for further tests that could provide clearer evidence of its efficacy and safety.
Selman Waksman (middle) in his laboratory, sorting through soil samples with two unidentified assistants. Credit: National Museum of American History
Its effectiveness in humans was still unknown, however. In 1944, amid unfinished animal experiments, the clinic decided they had nothing to lose in testing the drug on Patsy Thomas, a young, dying woman with a TB-riddled lung. By the end of her five-month course of streptomycin, Thomas’ illness had faded until it affected only a small region of one of her lungs, which surgeons then removed. Thomas became the first in a long line of people to fully recover from TB with the aid of medicine. In 1952, Waksman won the Nobel Prize in Physiology or Medicine for his discovery.
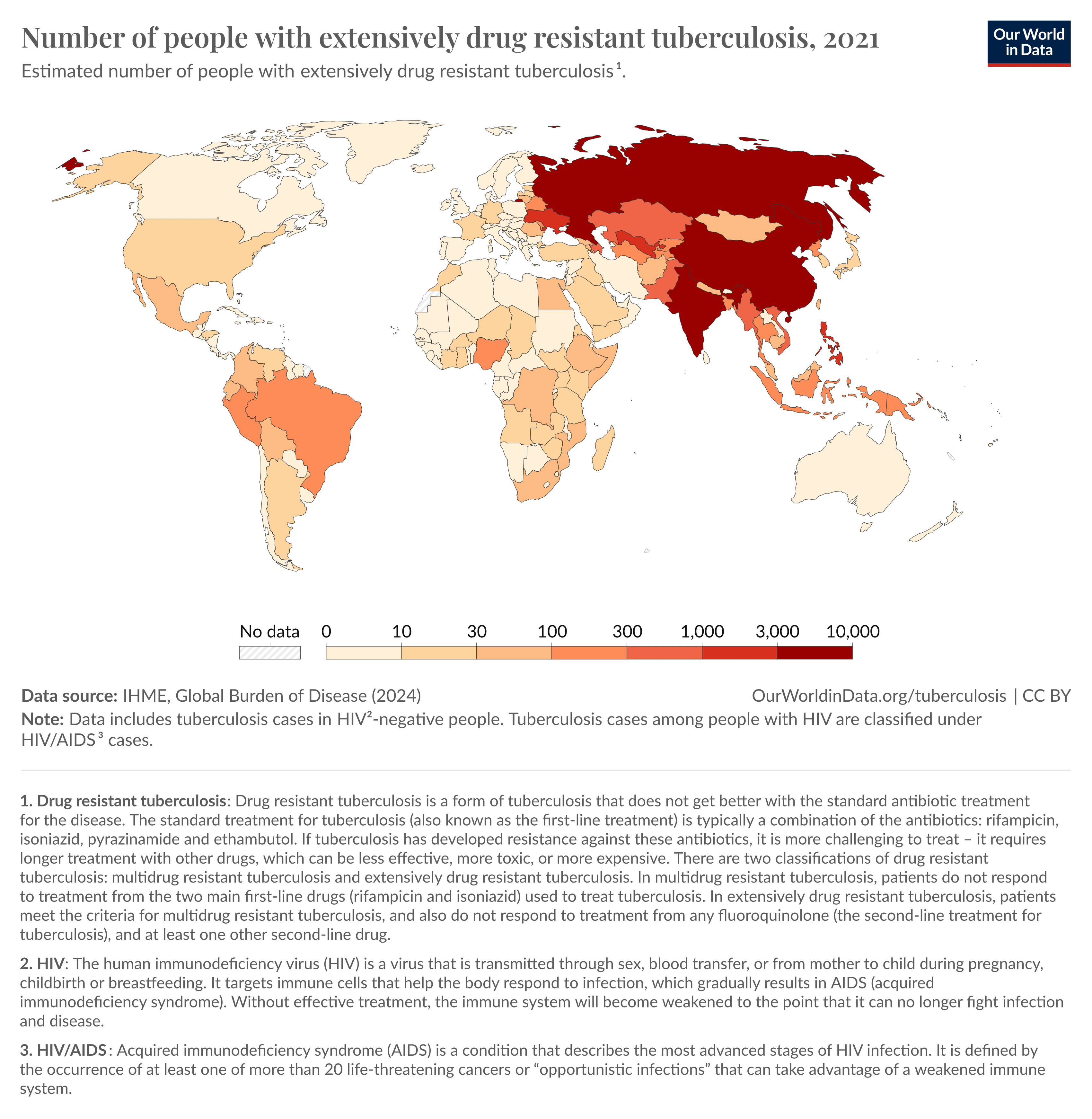
Unfortunately, a problem with streptomycin soon surfaced. M. tuberculosis strains mutated and developed resistance to the drug when administered as a single antibiotic. Physicians began prescribing multiple antibiotics to each patient so that bacteria resistant to one antibiotic would still be thwarted by the others. Even so, resistance continues to rise today, with some extensively drug-resistant strains unassailable using at least four of the most common and effective TB antibiotics. These antibiotic-resistant strains today account for 2.5 percent of cases worldwide.
Another hurdle is that to cure TB, patients must take a variety of antibiotics daily for several months. Some of the second-line antibiotics used to treat resistant TB are much harsher and more likely to cause side effects. The CDC reports that these can vary from mild symptoms, such as tingling, numbness, or loss of appetite, to severe problems, such as fever, vomiting, and blurred vision. Some fluoroquinolones — a class of antibiotics that inhibits DNA replication — may even cause psychosis. Altogether, such side effects could dissuade patients from taking their medication as prescribed, and patients failing to complete their treatment create opportunities for the bacteria to evolve resistance.
These challenges have led to strategies such as directly observed therapy (DOT), in which nurses or physicians monitor patients to ensure they take their medicine every day. Nurses meet with patients daily, in person, or — in areas with electricity and access to technology — watch them take their pills via an online video call. In either case, DOT strains local healthcare providers.
Antibiotic resistance is a growing concern for nearly all bacterial infections. It is responsible for over one million deaths per year (and is projected to rise ten times over by 2050). M. tuberculosis’ cellular architecture, however, presents an additional challenge for scientists developing new antibiotics.
Most bacteria harbor a cell wall made of the carbohydrate peptidoglycan, but M. tuberculosis modify their peptidoglycan to be unusually thick and water-repelling. In this form, it shields the pathogen’s cells from many common antibiotics, including broad-spectrum β-lactams. Since the cell’s outer armor slows down the entry of antibiotics, several drugs used to treat M. tuberculosis operate by tearing down the wall, including isoniazid and ethambutol. Drugs that have been tested on other types of bacteria often can’t be used to treat drug-resistant M. tuberculosis infections because of this distinction.
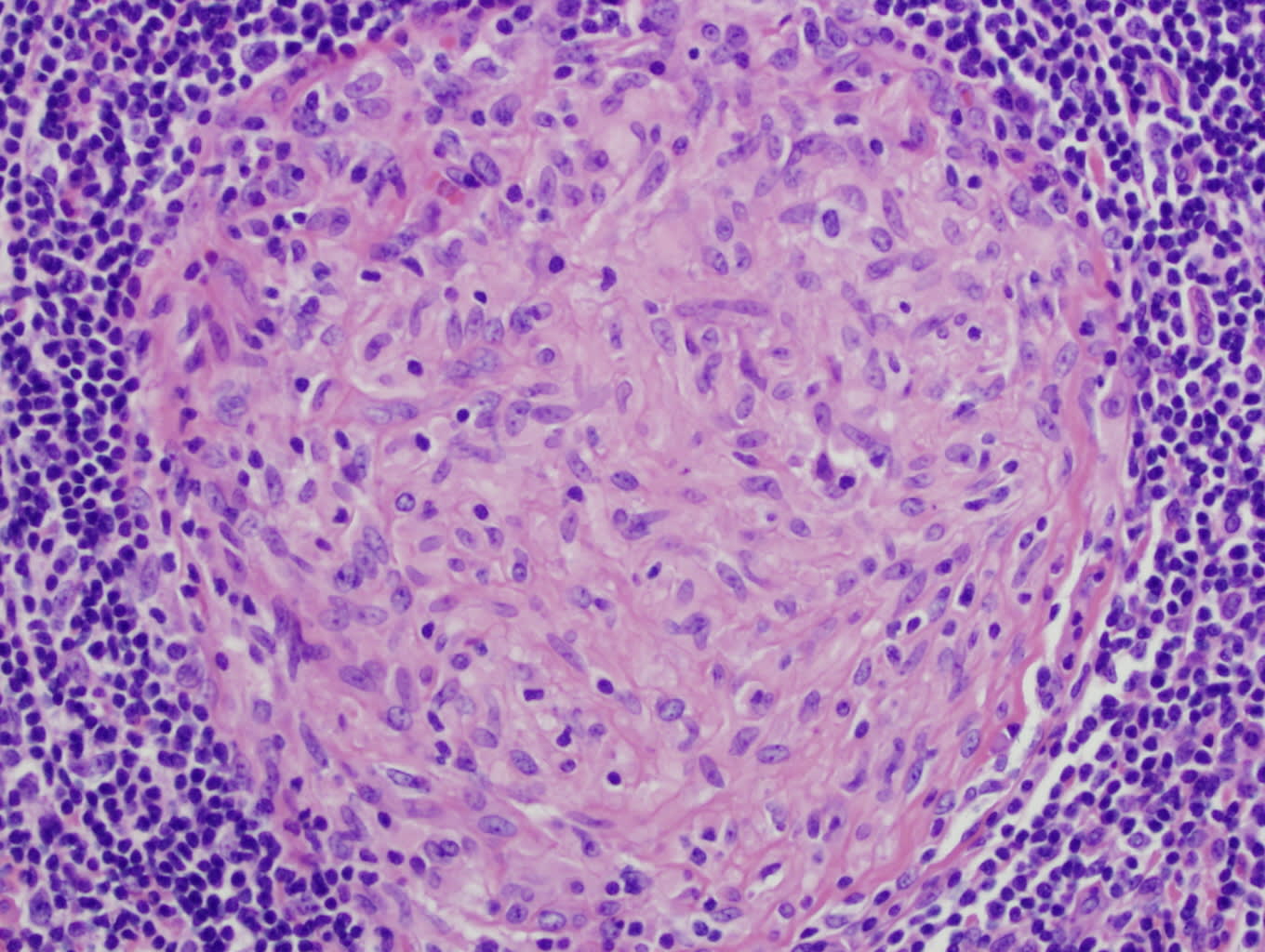
The thick wall around the bacterium isn’t the only barrier to entry for antibiotics, either. The very shape of Mycobacteria also presents a challenge; they look like long rods and cluster together to form “cords.” The bacteria also cluster sideways, thickening the cords, and making it so any bacteria sheltering near the middle of the cluster are shielded from drugs. When M. tuberculosis enters a human cell, large cells called macrophages engulf and break them down, surrounding the pathogens and forming a clump known as a granuloma. Not all pathogens are killed by the macrophages, however, and those that survive within the granuloma’s center fail to be cleared by antibiotics.
A granuloma found inside an infected patient’s lymph node.
What’s more, microbiologists don’t fully understand the molecular mechanisms that underlie M. tuberculosis’ resistance. During the internship in which I worked on TB, I characterized one of the bacterium’s many poorly understood genes. By inserting the gene into a harmless, related species called M. smegmatis that already harbored its own copy, I overexpressed the gene to see if it supplied the microbes with additional resistance. Testing the engineered cells against four common drugs, I found that the M. smegmatis overexpressing this little-known gene was able to withstand one of the first-line antibiotics — for reasons that remain unclear even now.
The gene I studied represented a single variant that protected the bacteria from antibiotics, but other gene variants could render these microbes more susceptible to antibiotics. Researchers today are often unaware of which gene variants confer antibiotic resistance, though, and physicians continue treating patients with antibiotics that introduce selection pressures on M. tuberculosis strains. Over time, the frequency of resistance gene variants in the population will continue increasing because only the bacteria lacking those variants will die with treatment.
A Rival Vaccine
With a vaccine that doesn’t guarantee protection and drugs that become ineffectual as bacteria evolve, researchers must develop new preventatives and therapies to control TB.
In 2018, GlaxoSmithKline (GSK) piloted a new vaccine that may outmatch the BCG vaccine in treating pulmonary TB in adults. The vaccine, called M72/AS01E, showed promise partly because its formula contains new chemical adjuvants that more effectively prime the immune system, including QS-21, a plant saponin cultivated from the Chilean soapbark tree Quillaja Saponaria, and monophosphoryl lipid A (MPL), a lipid found in bacterial membranes.
A phase 3 clinical trial for M72/AS01E, funded by the Gates Foundation, began this year. The Gates Medical Research Institute is running the trial in several nations where TB is widespread, such as South Africa, Zambia, Malawi, Mozambique, Kenya, Indonesia, and Vietnam.
While the phase 3 trial is ongoing, data from a previous, phase 2b trial offers some insight into the new vaccine. The trial runners reported some safety issues, for example; while only 45.4 percent of participants receiving the placebo reported at least one symptom, the proportion was 67.4 percent for those receiving the shot, including injection-site swelling and pain, as well as flu-like symptoms such as fever, fatigue, headache, malaise, and muscle aches. The phase 2b trial included 3,573 participants, whereas the phase 3 trial will include around 20,000; enough that the vaccine’s developers could detect rarer side effects.
Although side effects were prevalent in the phase 2b trial, this new vaccine might boast better safety than the BCG shot. Unlike the live-attenuated vaccine, M72/AS01E is composed of two M. tuberculosis antigens rather than whole bacteria. In principle, this makes it safer to administer to people with undiagnosed HIV infections, for instance, who might struggle to clear live microbes out of their system.
While the new trial could provide valuable information about the vaccine’s safety, the study design may limit insight into its efficacy. As is commonplace for many clinical trials, the control arm takes a placebo — a sham vaccine consisting of no more than sugar dissolved in an inert buffer. However, this experimental design will only reveal whether the vaccine works better than a placebo. What truly matters is how it compares to the existing BCG vaccine. For that, we need a direct comparison between the two options. The trial runners favored a placebo over the existing vaccine during the phase 2b trial, noting that most of the participants had received the BCG vaccine in the past. However, since the efficacy of the BCG vaccine wanes over time, a booster dose may offer protection and serve as a better comparator.
Past research underscores the importance of comparing new candidates to existing immunizations. Researchers in 2018 tested out another TB vaccine, called H4:IC31, against two control groups — a placebo arm and an arm receiving a BCG booster. Researchers dropped work on H4:IC31 when they discovered that, although it worked better than the placebo, it paled in comparison to BCG revaccination.
Although it is worth confirming that M72/AS01E is effective by testing it against a placebo, researchers may decide not to pursue it further if, like H4:IC31, it does not measure up to the BCG vaccine and bears few other advantages. For instance, in the same way that the BCG vaccine requires refrigeration, so does the new vaccine, meaning the new shot would face similar challenges in reaching remote parts of the globe.
Ultimately, the phase 2b trial showed that M72/AS01E afforded protection against active, pulmonary TB in 50 percent of the participants in the experimental arm. However, a direct comparison between the two vaccines is still needed to offer a clearer picture of their relative strengths.
OK, Computer. Find Antibiotics
Scientists use two different strategies to discover new treatment options for TB. One involves using computer models to sift through chemical databases in search of compounds that may have antibacterial properties. The other centers around screening compounds against bacteria to study their mechanisms of action and work out which drug combinations are most effective.
Traditional drug discovery has been a time-consuming, resource-intensive process involving the synthesis of thousands of chemicals, weighing their efficacy, and profiling their safety. But now, researchers are increasingly using machine learning to speed up pharmaceutical breakthroughs.
One research team at the Massachusetts Institute of Technology developed a machine learning algorithm to rapidly find drugs that could thwart a different bacterium: Escherichia coli — a food-borne pathogen that causes diarrhea. In the process, they discovered a broad-spectrum antibiotic that might just work on M. tuberculosis.
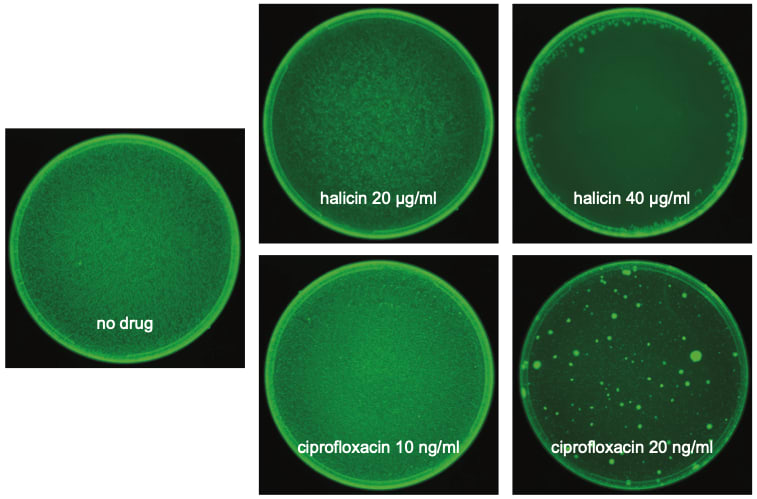
Their algorithm works by discerning which chemical structures are likely to inhibit E. coli bacteria from growing. To train their model, they used a selection of over 2,000 compounds from a U.S. Food and Drug Administration (FDA)-approved drug library, some of which inhibit E. coli. The researchers then tested their model by feeding it 6,000 molecules from the Drug Repurposing Hub, and seeing which ones the model predicted might elicit anti-bacterial effects. Researchers experimentally validated the top 99 hits, finding that 51 inhibited E. coli growth. To narrow their focus, they prioritized those molecules that had already undergone multiple phases of clinical trials, because they have the most data confirming their safety. They zeroed in on halicin, a drug with broad-spectrum potential that had previously been trialed to treat diabetes but proved inefficacious in that regard.
E. coli plated onto media containing halicin or ciprofloxacin antibiotics, after 7 days of incubation. Credit: Stokes J.M. et al. Cell (2020).
Halicin kills microbes faster than other antibiotics used to treat TB. When M. tuberculosis is cultured in lab media with halicin, for example, the drug kills the microbes within 24 hours; the bacteria cannot reproduce quickly enough to replenish the population. Scientists must next perform in vivo experiments in animal models to assess how quickly halicin kills the pathogen in a more physiologically relevant setting, such as within a granuloma that shelters bacteria from antibiotics. Promisingly, halicin worked in a mouse model for Acinetobacter baumannii, another bacterial threat conferring resistance to many antibiotics.
Halicin isn’t the only repurposed drug that could treat TB, either. Pharmacologists have also applied machine learning to find five antimalarial drugs with similar TB-fighting potential. Many more could emerge as machine learning tools improve.
Another approach to discovering antibiotics involves using machine learning in parallel with scaled-up laboratory experiments. The primary screening of strains to prioritize expanded chemistry and targets (PROSPECT) tool, developed by biologists at Harvard University, rapidly finds compounds that target specific bacterial proteins. The protocol involves generating 474 mutants of M. tuberculosis by removing important genes, thus rendering them hypersensitive to drugs compared with bacteria equipped with a full genome. The researchers then subjected these mutants to over 3,000 different compounds, measuring how well each one killed off various mutants to build a dataset with millions of correlations between chemicals and genes. To whittle these down to a few interesting hits, they used a machine learning model trained to detect which interactions between compounds and bacterial proteins are likely to elicit a therapeutic effect based on existing therapies.
The researchers were left with 40 drug candidates. These targeted different bacterial components, including RNA polymerases that control gene expression plus enzymes involved in synthesizing the bacterium’s unique cell wall. The most alluring compounds target bacterial components that previous drug discovery efforts missed, including an efflux pump called EfpA that recent research shows may confer resistance to frontline antibiotics, namely isoniazid, by expelling them from inside the cell.
The value of machine learning extends beyond finding new antibiotics or repurposing old drugs. It can also help scientists rapidly uncover the mechanism of action for entirely new drug candidates.
The morphological evaluation and understanding of stress (MorphEUS) algorithm is a machine-learning driven imaging platform that deciphers which biological pathways a drug targets based on morphological changes to the cell, such as the shape of its DNA nucleoid or the integrity of its cell wall. For example, MorphEUS can detect that antibiotics like ethambutol and isoniazid break down the cell wall by measuring how it grows thinner over time. Researchers used this tool to classify the molecular pathways targeted by 37 antibiotics.
As researchers identify new drug candidates to treat TB, they must also work out how effective they are when paired with other antibiotics in combination therapy. And the number of combinations that researchers can test is growing rapidly.
There are over 23,000 ways that scientists can group the existing 28 TB drugs into combinations of three or four antibiotics. Instead of experimentally validating all these combinations, researchers developed an AI model called inferring drug interactions using chemogenomics and orthology (INDIGO) to predict whether combined drugs synergize or antagonize each other. Their model leverages data on how each drug performs alone at inhibiting M. tuberculosis growth and uses transcriptomic data from each drug to determine drug-gene interactions.
Using INDIGO, researchers found that some drug combinations work better than others, and some cancel out each other’s effects. In general, drugs that inhibit bacterial growth amplify each other’s impact when mixed together, but bacteria-killing drugs tend to mesh poorly when paired with other antibiotics. As new drugs pour in, this tool could help predict which drug combinations maximize impact.
Scientists at Obafemi Awolowo University in Nigeria are also searching for drugs that complement and enhance current antibiotics, but without using machine learning. They have already shown, for example, that statins such as atorvastatin, which normally lower “bad” cholesterol, may also help antibiotics diffuse across the cholesterol layer on the surface of M. tuberculosis. Rather than producing their own cholesterol, the pathogen sequesters these molecules from the host, so the effectiveness of these statins could be linked to lowering overall cholesterol levels in the body. Many people with TB struggle to commit to long-term treatment programs, so the boost in efficacy that statins provide to antibiotics could lead to shorter treatments overall.
In the end, incentivizing patients to take their medicine as prescribed — or finding ways to shorten treatment plans — could prove just as important as finding new antibiotics.
Can We Lay This Scourge to Rest?
When I interned in the TB laboratory as a biology student intrigued by infectious diseases, I knew very little about this condition. My classes had focused on flu, polio, and other pathogenic threats, but TB took up little attention; so you can imagine my surprise when I learned I had joined a research group striving to take down the world’s greatest infectious killer. But what has become a forgotten pandemic in developed, Western countries pervades the lives of many people in Sub-Saharan Africa and South-East Asia.
Excited as I was to contribute to TB research, I grew disillusioned by the pharmaceutical industry’s indifference to it.
Despite the initial promise of GSK’s M72/AS01E vaccine, the company chose to pivot to a more lucrative shingles vaccine that used the same adjuvants despite their short supply, thereby stalling research into the new TB vaccine until a decade later, when the Gates Foundation began funding the phase 3 trial.
Similarly, even in the face of the growing threat of drug resistance, research has moved away from antibiotic discovery efforts to explore more profitable medicines. Developing and launching a new antibiotic costs $1.5 billion U.S. dollars, whereas cancer therapies require only $640 million to make overall. Antibiotics also rake in less revenue, approximately $46 million per year, as compared to cancer treatments ($1.7 billion per year), leaving big pharma with little incentive to focus on this forgotten pandemic. TB researchers often find themselves frustrated to realize that we may never control this global burden as long as big pharma lacks the financial incentive to take up research on less profitable but widely neglected therapies.
However, hope prevails. We have controlled other bacterial pests once common in the developing world through the top-down work of health agencies and drug developers and the bottom-up efforts of local volunteers. Back in the 1950s, 50 million people used to suffer from yaws, a disfiguring skin disease caused by Treponema pallidum pertenue, a close relative of the syphilis bacterium. That number shrank to approximately 223,000 cases by 2023. Mass treatment campaigns have also quelled Mycobacterium leprae, a relative of M. tuberculosis that causes leprosy. Global cases of leprosy dropped from over 5.2 million in 1985 to 250,000 today thanks to antibiotic treatment efforts.
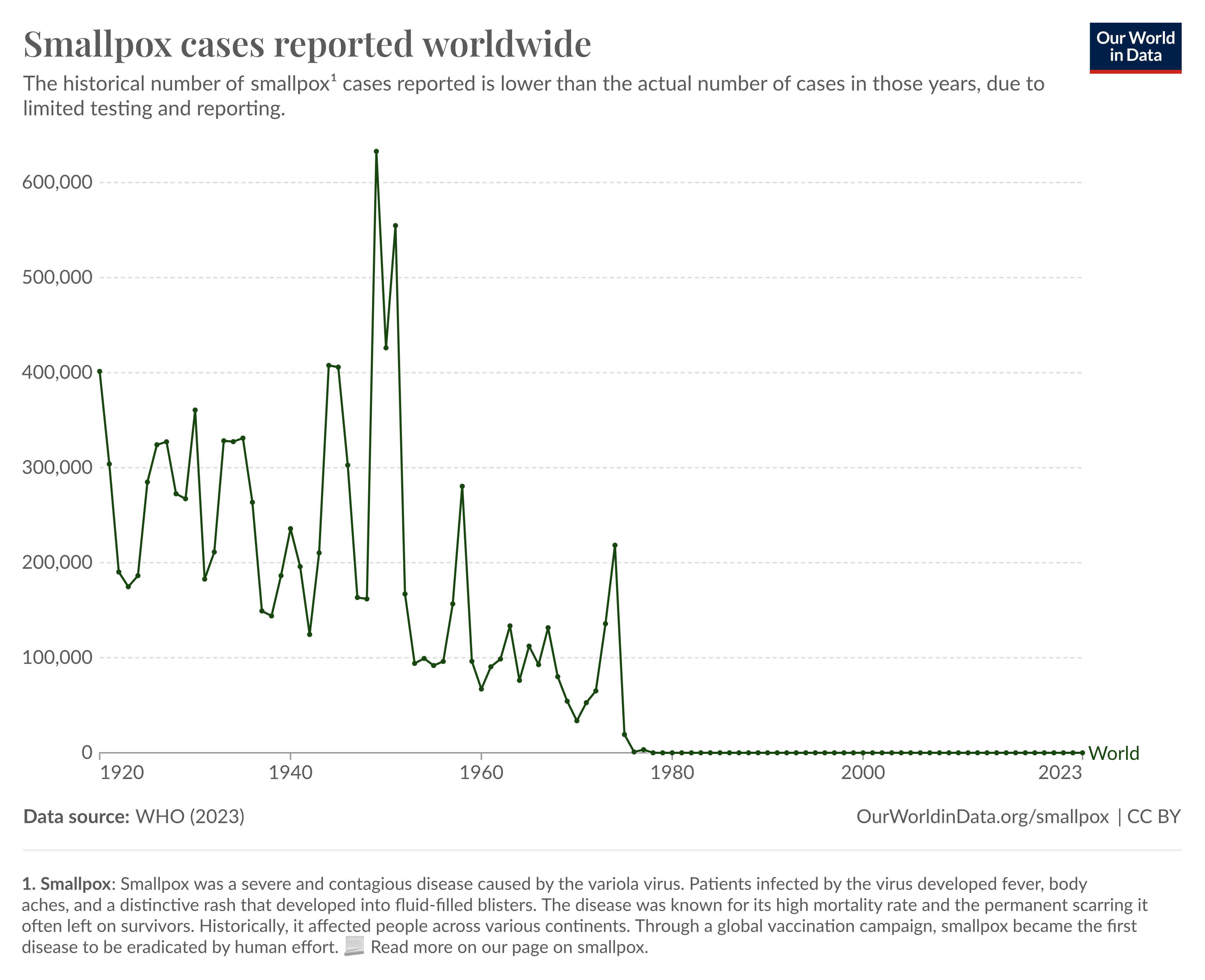
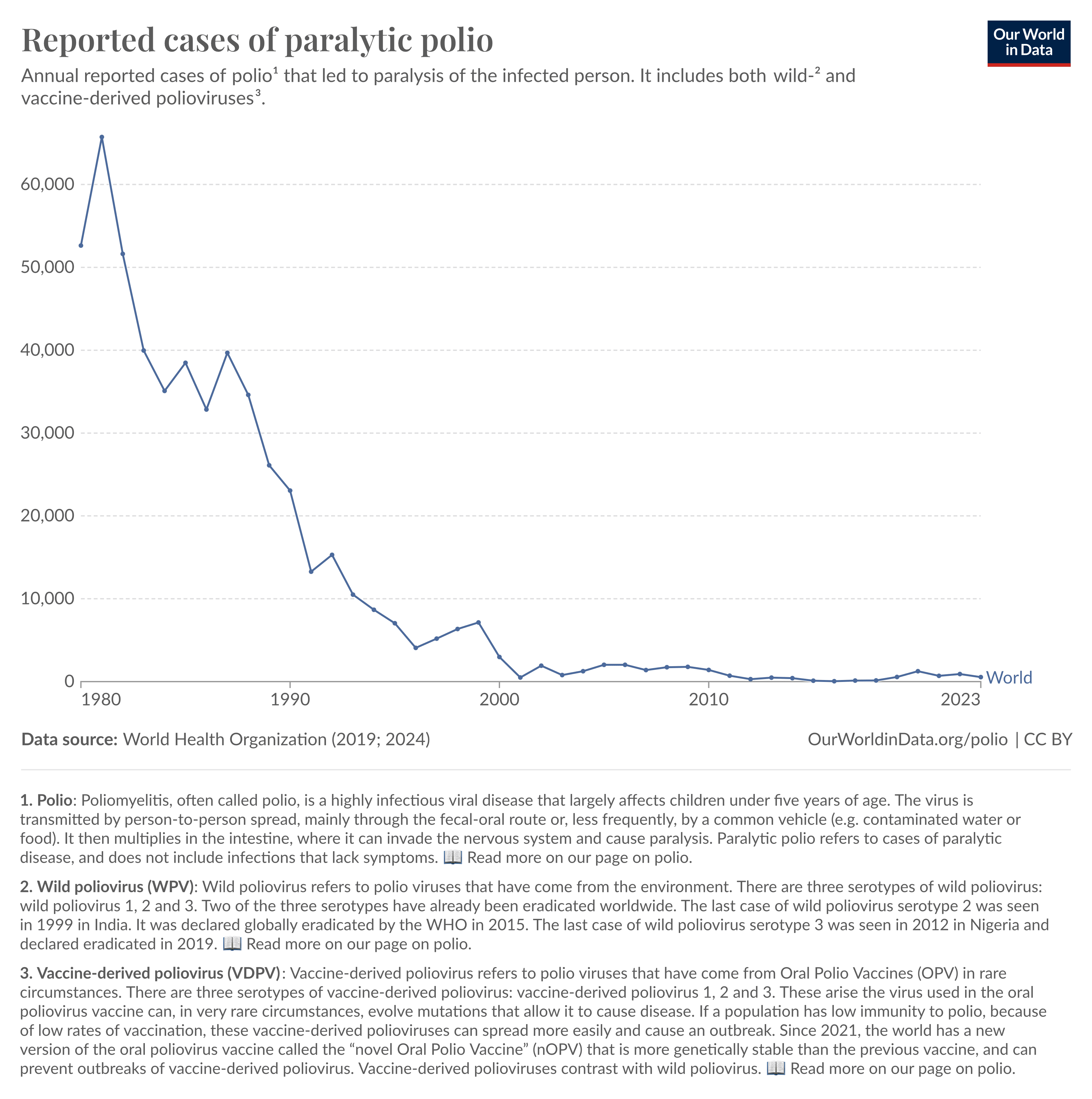
While TB presents a larger challenge than either of these bacteria due to the sheer abundance of cases, our history of stamping out viral pandemics offers reassurance. Effective vaccines subdued polio, giving it a near-eradicated status today,4 as well as smallpox, the first human pathogen to become completely extinguished.
I remain optimistic that the recent advances could drive major breakthroughs in tackling M. tuberculosis. The new vaccine purportedly offers better protection against the respiratory form of the illness, and machine learning innovations have bolstered antibiotic discovery campaigns, bringing several new candidates to light. And even more fundamentally, repurposing old drugs with good safety profiles could allow the industry to save on cost, encouraging them to shift their focus to TB therapies.
We’ve come a long way from treating TB patients by removing their ribs or pumping nitrogen into their chest cavity. If written today, The Magic Mountain would surely present the illness in a different light, extolling all that vaccines and drugs have done to mitigate suffering. Hopefully, diagnostics and interventions currently in development, as well as those on the verge of discovery, can bring us closer to the day TB takes its last breath.
***
Kamal Nahas is a researcher-turned-journalist based in Oxford, UK, who covers stories in biology, health, and technology.
Thanks to Jacob Trefethen for proposing the essay idea and providing resources; Devon Balwit, Xander Balwit, Saloni Dattani, Niko McCarty, and Merrick Pierson Smela for editing drafts of this essay.
Cite: Nahas, Kamal. “The Long Road to End Tuberculosis.” Asimov Press (2024). DOI: https://doi.org/10.62211/85pr-22fg
***
Footnotes
- Potatoes were not rationed initially, but as the war intensified they were issued in quantities varying from two to six pounds per person. Ox bile wasn't rationed, but under German occupation, it was difficult to obtain from the slaughterhouse.
- Data on vaccinations or vaccine provisions are not available for every country, such as French Guinea, Iceland, parts of Sudan, Suriname, and Western Sahara. In some developed countries where TB incidence is low, such as the U.S., BCG vaccination is only recommended for at-risk individuals, such as children of TB patients.
- Albert Schatz, who first isolated streptomycin, felt that his supervisor, Waksman, did not properly acknowledge his contribution to the discovery of the antibiotic. He later sued Waksman, claiming 3 percent of the royalties and $120,000 in foreign patent rights. He even tried petitioning the Nobel committee to retroactively include him in the award, but they didn’t budge.
- In the case of polio, ineffective vaccines are part of the problem because attenuated viral vaccines can mutate back closer to wild-type and regain virulence.



Executive summary: Despite significant progress, tuberculosis remains the deadliest infectious disease globally, killing 1.2 million people annually, but new vaccines, antibiotics, and drug discovery methods offer hope for meeting ambitious goals to reduce TB cases and deaths by 2030.
Key points:
This comment was auto-generated by the EA Forum Team. Feel free to point out issues with this summary by replying to the comment, and contact us if you have feedback.