This is a summary of a report on perinatal mental health, created by Stan Pinsent of CEARCH on behalf of the Flourishing Minds Fund. CEARCH is a philanthropic research and grantmaking organization, identifying highly impactful philanthropic causes and working to support them with additional funding and talent.
Perinatal mental illness, primarily depression and anxiety, affects an estimated 10-20% of pregnant women and new mothers globally. It is linked to increased rates of stillbirth and preterm birth, and can impair the mother's ability to bond with and care for her child. It may cause developmental problems in the infant that persist into adulthood.
While afflicted, women experience low mood, low self-esteem and an elevated risk of self-harm and suicide. Widespread stigma around mental illness means that these women often suffer in silence.
The burden is slightly higher in low- and middle-income countries (LMICs), disproportionately affecting vulnerable and disadvantaged women. Although there is unmet need everywhere, low-income countries typically have 50x fewer mental health professionals per capita than high-income countries, and perinatal mental illness often goes completely ignored. This, and the lower cost of providing treatment in these countries, means that most of the promising opportunities are in LMICs.
Recent decades have seen significant improvement in Maternal and Neonatal Health (MNH) outcomes, but not in Perinatal Mental Health (PMH). We expect PMH to continue to grow as a share of the health burden in LMICs .
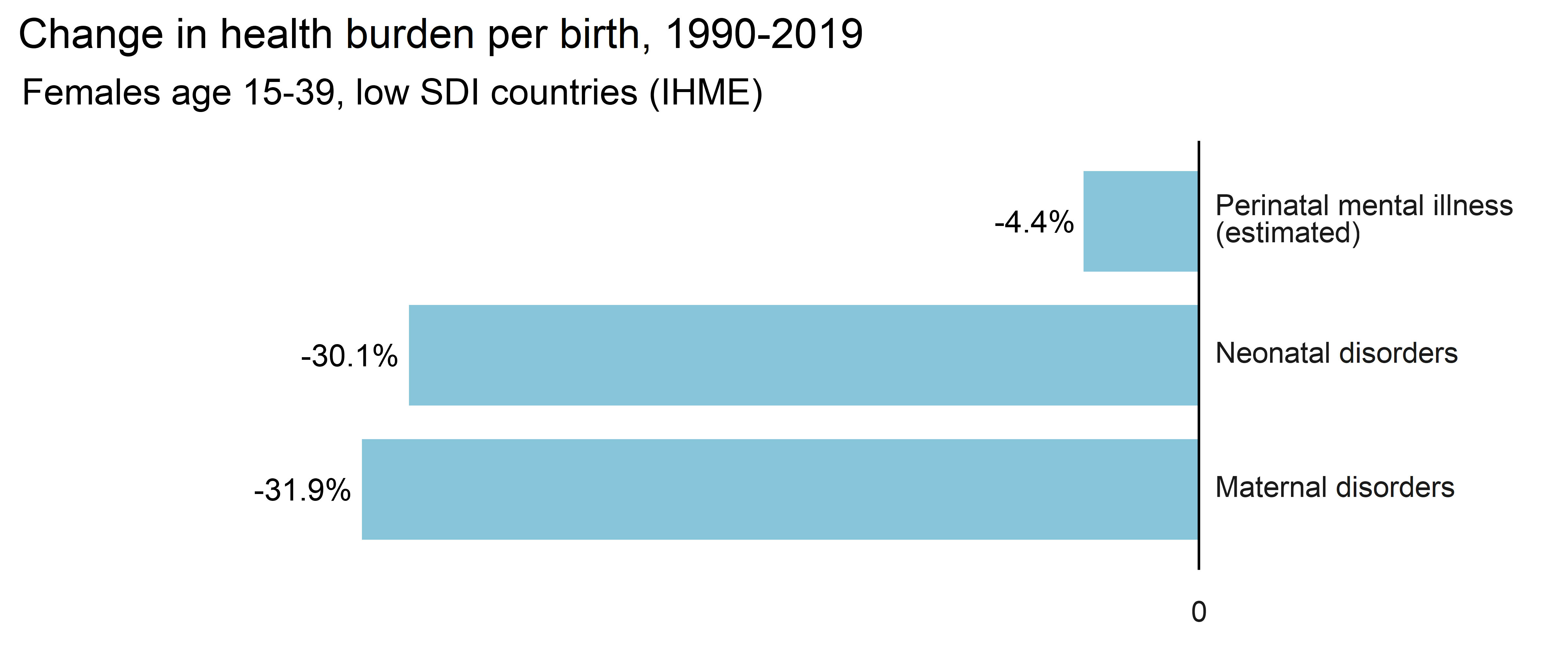
Fig. 1: The burden of perinatal mental illness is decreasing more slowly than other maternal and neonatal disorders[1].
Layperson-delivered Interpersonal Group Therapy (IPT-G) is widely considered to be an effective way to scale-up access to mental health treatments in low-income countries, and probably has a role in tackling perinatal mental illness. There are also opportunities to improve physical and mental health in tandem, such as through Participatory Action and Learning (PLA) groups, which can bring communities together to share knowledge and to support mothers. It has been claimed that when well-attended, these community interventions can avert maternal and infant deaths for around $1,000 each[2].
Interventions in this space face the challenge of reaching pregnant women and mothers who are often physically and socially marginalized. This can be done by:
- Attaching to existing services like midwife care or anti-poverty programs to engage women in hard-to-reach places. Grant funding can help to scale up such approaches or fund studies on the effectiveness of new initiatives.
- Utilizing technology. Internet access is spreading rapidly, increasing the feasibility of interventions like self-help apps or online psychotherapy. Apps and online courses can train health care workers to identify and treat perinatal mental illness. We are optimistic that well-directed grants could advance organizations in this space from concept to impact.
- Preventing Intimate Partner Violence (IPV) through “edutainment” campaigns or by pushing for improved women’s property rights. This is a largely untested space which could prove to be a major lever in preventing perinatal mental illness.
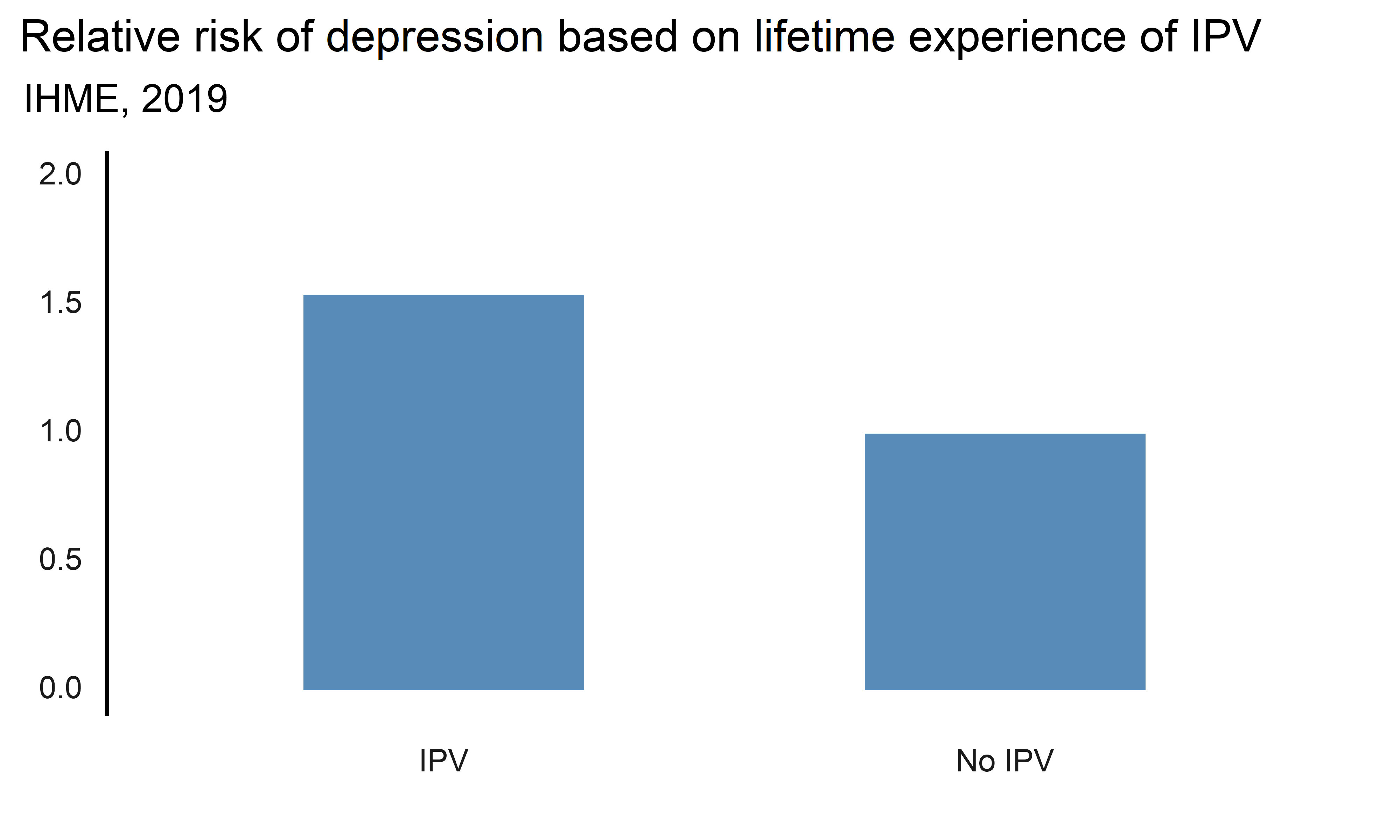
Fig. 2: IHME estimates that women who have experienced IPV at any point in their life are 1.54x more likely to experience major depressive disorder.
There may be opportunities for small, high-impact research grants of $100k-$200k that contribute to the global effort to improve PMH. We are particularly excited to see:
- Research on the effectiveness of new treatments
- Efforts to determine the secondary effects of mental health interventions on child development and on maternal outcomes beyond mental health.
- Analysis that informs future grantmaking by addressing some of our key uncertainties.
This report is the first stage of a process that will conclude with a seven-figure grant portfolio to address perinatal mental illness.
The full report on perinatal mental health can be found here.
A summary of my previous report on mental health interventions can be found here.

This is great work Stan, as a former religious network builder, now not religious and entering the space of scaling of lay-therapy in LMICs, I can see developing partnerships with religions and parachurch networks in LMICs to give use of their properties for community Mental Health Care (MHC), as well as helping them further their own versions, usually called spiritual counseling, in line with good science. In the USA this marriage is common and a significant percentage of the total MHC given the entire US population is done by religious org's, a reality not well understood by secular professional communities. This won't be my main modality, but leave no stone unturned.
I'm interested in many new therapeutic methods not even included in your report, that are just yet to be invented or perfected. I'm excited about the recent Australian BMJ Meta Analysis of Exercise interventions for depression that found dance to be more effective than any of the exercise types, as well as beating both SSRI's and CBT...unfortunately a small sample size that needs more study, but still amazing. We will certainly run pilots on that in our new work.
Jeffrey Kursonis