Summary
Immediate skin-to-skin contact (SSC) between mothers and newborns and early initiation of breastfeeding (EIBF) may play a significant and underappreciated role in reducing neonatal mortality. These practices are distinct in important ways from more broadly recognized (and clearly impactful) interventions like kangaroo care and exclusive breastfeeding, and they are recommended for both preterm and full-term infants.
A large evidence base indicates that immediate SSC and EIBF substantially reduce neonatal mortality. Many randomized trials show that immediate SSC promotes EIBF, reduces episodes of low blood sugar, improves temperature regulation, and promotes cardiac and respiratory stability. All of these effects are linked to lower mortality, and the biological pathways between immediate SSC, EIBF, and reduced mortality are compelling. A meta-analysis of large observational studies found a 25% lower risk of mortality in infants who began breastfeeding within one hour of birth compared to initiation after one hour.
These practices are attractive targets for intervention, and promoting them is effective. Immediate SSC and EIBF require no commodities, are under the direct influence of birth attendants, are time-bound to the first hour after birth, are consistent with international guidelines, and are appropriate for universal promotion. Their adoption is often low, but ceilings are demonstrably high: many low-and middle-income countries (LMICs) have rates of EIBF less than 30%, yet several have rates over 70%. Multiple studies find that health worker training and quality improvement activities dramatically increase rates of immediate SSC and EIBF.
There do not appear to be any major actors focused specifically on promotion of universal immediate SSC and EIBF. By contrast, general breastfeeding promotion and essential newborn care training programs are relatively common.
More research on cost-effectiveness is needed, but it appears promising. Limited existing evidence suggests that programs targeting these practices may be highly cost-effective. The most efficient programs will balance effect sizes with intervention intensity.
For readers interested in a deeper look at the evidence, our extended report is available here.
We welcome feedback, suggestions, and ideas! Feel free to leave a comment or send us a direct message in the forum if you’d like to chat.
Introduction
In this report we discuss a promising approach to address neonatal mortality through two closely-related practices that should occur within the first hour after birth: immediate skin-to-skin contact (SSC) and early initiation of breastfeeding (EIBF). Immediate SSC involves placing a newborn directly on the mother’s bare chest or abdomen within 10 minutes of birth and maintaining contact for at least one hour or until the first breastfeeding is complete, and EIBF refers to starting breastfeeding within one hour of birth. Both are among the key practices recommended for all newborns by the World Health Organization (WHO) and UNICEF [1].
Immediate SSC and EIBF are distinct from kangaroo care (KC; also known as kangaroo mother care or KMC), an intervention targeted at preterm and/or low birthweight infants[1] involving early and prolonged skin-to-skin contact along with breastfeeding promotion [2], and exclusive breastfeeding (EBF), or feeding infants only breast milk for their first six months [3].
While benefits of KC and EBF are broadly recognized among impact-focused organizations[2], universal promotion of immediate SSC and EIBF for all newborns may be underappreciated[3]. There are several reasons that immediate SSC and EIBF may be especially promising:
- There is a large evidence base supporting these practices independent of longer-term behaviors such as KC or EBF.
- Some of their mechanisms may be unique to their very early timing after birth - a window of opportunity where health workers are often present and could strongly influence behaviors.
- They are recommended practices for all births (unlike KC, which targets a subset of higher risk infants), making them appropriate for universal adoption, which could simplify their promotion and implementation.
- They require essentially no additional resources, carry negligible risks, and are already broadly recommended by international and national health guidelines.
- They appear to be practiced very inconsistently, and targeted efforts to raise rates have been highly successful - yet few actors are scaling these efforts.
A. The burden of neonatal mortality remains large, and much is preventable
Rates of child mortality are extremely skewed towards the first few days of life. Over a third of all deaths under the age of five occur within the first week of life and 39-47% within the first month (the neonatal period) [4], [5], [6]. There are approximately 2.4 million neonatal deaths annually - equivalent to over 6,500 per day - and neonatal disorders are among the top three causes of disability-adjusted life years globally [7]. Despite considerable progress in reducing infant mortality rates over the past few decades, over half of neonatal mortality is still felt to be preventable with basic and low-cost care [8], highlighting an urgent and ongoing need to promote effective practices.
B. Immediate SSC and EIBF appear to reduce neonatal mortality
Immediate SSC and EIBF are closely related: EIBF necessarily involves a degree of skin contact, and immediate skin contact strongly promotes early breastfeeding: in a cross-sectional observational trial involving 1,383 births in eight countries, the duration of uninterrupted SSC initiated within one minute of birth was found to have a strong dose-response relationship with EIBF [9].
Several strands of evidence[4] come together to strongly suggest that these practices reduce neonatal and infant mortality. We start by reviewing the observational evidence for EIBF, proceed to a discussion of the experimental evidence for immediate SSC, and examine the pathways (both shared and independent) through which they could impact health outcomes.
EIBF is associated with reductions in mortality in large observational trials
Several large cohort trials [10], [11], [12], [13] from Ghana, Tanzania, India, and Nepal, established a strong association between the timing of breastfeeding and neonatal mortality.
These studies were conducted between 1998 and 2014 and included between 10,000 and 100,000 infants. Their findings were remarkably consistent: in the three cohorts that examined breastfeeding initiation at <1 hour [10], [11], [12], delayed initiation from 1-24 hours was associated with a 32-43% increased risk of mortality after adjustment for confounders. Delays of over 24 hours, compared with <1 hour, were associated with at least a 78% higher risk of neonatal death in each of these studies. Only two studies [12], [14] examined mortality past 28 days, but the association seemed to persist up to six months of age. The first, much larger (n=99,632) and higher-quality study found that mortality rates remained 34-48% higher from 28 days to 6 months in infants who initiated breastfeeding after one hour.
All studies used regression analysis to adjust for expected confounders[5]. Two studies [10], [12] also adjusted for the subsequent pattern of breastfeeding and found that EIBF was associated with lower mortality regardless of whether neonates continued to be exclusively breastfed[6].
Perhaps the most intuitive alternative interpretation of this association (i.e., other than that early breastfeeding reduces mortality) is that newborns born in poor health are both less likely to breastfeed early and more likely to die. To help address this possibility of “reverse causation”, all studies excluded deaths occurring within the first 1-4 days in their main results. Additionally, two studies [11], [13] performed secondary analysis excluding infants with evidence of severe illness within the first 48 hours, and one study [10] repeated analysis excluding infants who were unwell at birth, had congenital abnormalities, or died in the first week. In all cases the EIBF-mortality association persisted with little or no attenuation.
Despite a number of uncertainties with these studies[7], we feel the association between EIBF and decreased neonatal mortality is convincing and supports a causal interpretation. In particular, causality is supported by the strength of the association, which seems unlikely to be fully accounted for by reverse causation or confounding factors, and the strong biological plausibility that EIBF could reduce neonatal mortality through several pathways which experimental evidence supports: particularly through its close association with SSC.
Experimental evidence shows that SSC improves important clinical outcomes
A large body of randomized evidence demonstrates that SSC improves many clinical outcomes which are likely to reduce neonatal mortality.
Well-established benefits of immediate and/or early SSC[8], derived from meta-analysis of RCTs [15], [16], [17], include greater success and longer duration of initial breastfeeding episodes[9], increased rates of exclusive breastfeeding from birth to 6 months[10], decreased rates of hypoglycemia (low blood sugar)[11], decreases in both hypothermia and hyperthermia[12], and enhanced cardiac and respiratory stability[13]. Breastfeeding outcomes after cesarean births [17], [18] and measures of physiologic stress also appear to be reduced by SSC [19], [20], [21]. Meta-analysis [22] additionally shows that immediate SSC has benefits for mothers in reducing risk factors for postpartum hemorrhage[14] (PPH; an effect which is likely mediated by the hormone oxytocin).
We were not able to identify any randomized or high-quality observational trials evaluating SSC and mortality in full-term infants. However, the established mortality benefits of kangaroo care in preterm and/or low birthweight infants [23] suggests that the outcomes influenced by SSC have implications for neonatal survival.
EIBF and other outcomes of SSC are congruent with mortality benefits
The causes of neonatal death are often multifactorial. Through many well-established mechanisms, SSC and EIBF could plausibly mitigate the largest contributors to neonatal deaths: infections and complications of prematurity [24].
The available evidence also suggests that deaths averted by EIBF stem largely from reductions in infections [25], [26]. Exclusive breastfeeding (EBF) reduces infection-related morbidity in a limited number of randomized trials of breastfeeding-promotion interventions [27], [28], and the duration and exclusivity of breastfeeding is strongly linked to decreased mortality in numerous observational studies [29]. Early breastfeeding has the unique benefit of providing colostrum (the low-volume, thick, yellowish breast milk produced from birth up to approximately three days), which has concentrated amounts of components affecting immunity and gut development [30]. Breastfeeding additionally may decrease the risk of infection through early impacts on the microbiome [31], [32], while prelacteal feeding[15], which is associated with delayed breastfeeding, cessation of breastfeeding [33], and discarding of colostrum [34], could directly expose newborns to pathogens.
Several other benefits of immediate SSC are likely to support a mortality benefit. Colostrum from EIBF provides a source of nutrition, while SSC simultaneously reduces energy demands by reducing physiologic strains and providing warmth. Together this improves metabolic balance and may be reflected by the lower observed rates of hypoglycemia previously discussed. Hypoglycemia is linked by observational evidence to poor neurodevelopmental outcomes [35] as well as mortality [36]. Likewise, the relationship between newborn body temperature and severe adverse outcomes (including mortality) appears to follow a U-shaped pattern, with higher mortality risk in both hypothermic and hyperthermic states [37], [38]. Cardiac and respiratory instability, which is reduced by SSC, is very likely to be a predictor of mortality [39].
EIBF and SSC both seem to induce positive neurohormonal and behavioral feedback loops, including effects on the hormones oxytocin, cortisol, and prolactin [40]. Early breastfeeding and SSC also set the stage for the longer-term continuation of these beneficial practices.
Finally, postpartum hemorrhage is the leading cause of maternal mortality globally [41] and has obvious implications both for maternal and (indirectly) neonatal health outcomes. SSC could be particularly important to reduce postpartum hemorrhage when uterotonic medications such as oxytocin are delayed or not administered and/or where there is inadequate ability to respond to hemorrhage (such as in deliveries outside of medical facilities).
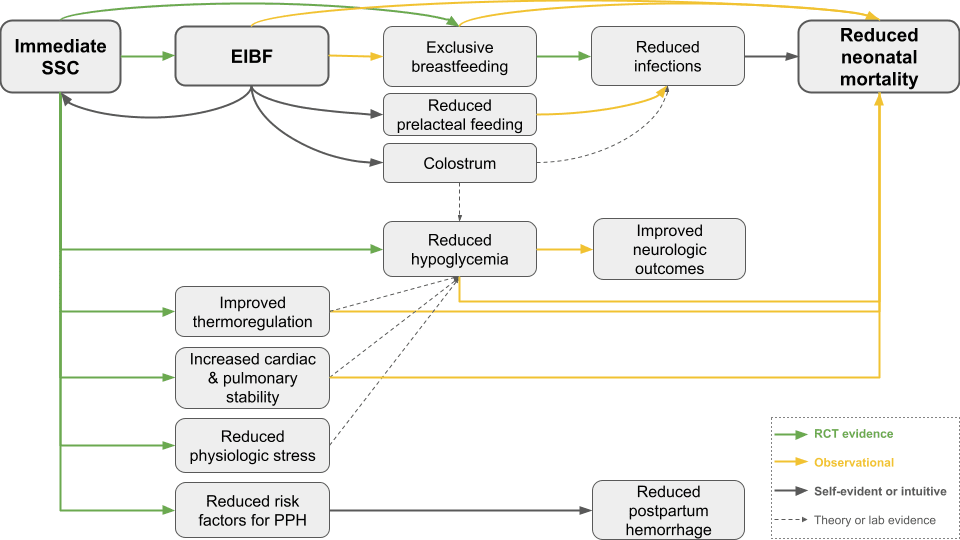
C. A visual summary of pathways from SSC and EIBF to impact
Figure 1. Visual summary of pathways between SSC, EIBF, and clinical outcomes. Type of evidence is indicated by color-coding of arrows.
D. The mortality benefit may be substantial, even with pessimistic assumptions
We don’t have randomized trial evidence to directly determine the degree of mortality reduction from immediate SSC or EIBF in full-term infants. However, we do not find the absence of RCT evidence to be problematic in this setting: running an RCT with statistical power to detect a mortality benefit in full-term infants, where neonatal death is much rarer than in selected high-risk populations (such as preterm or low birthweight infants), would have ethical concerns[16] and require enormous sample sizes[17].
The large cohort studies on EIBF [10], [11], [12], [13] we previously discussed can form a starting point for estimating the magnitude of the mortality benefit[18]. A meta-analysis which included data from all of these trials found that, compared to infants who initiated breastfeeding 1 hour after birth, infants who initiated breastfeeding 2–23 hours after birth had a 33% greater risk of neonatal mortality (95% CI: 13–56%), and infants who initiated breastfeeding 24 hours after birth had a 2.19-fold greater risk of neonatal mortality (95% CI: 1.73–2.77)[42].
Those figures exclude very early deaths (within 1-4 days of birth, depending on the underlying study) as a control against reverse causation, and do not include mortality estimates after 28 days[19]. Fortunately, the largest observational study on the EIBF-mortality association [12] (included in the meta-analysis) reports neonatal mortality data starting at day zero, and relative risks are very similar whether early deaths are included or excluded[20]. The same study also found that breastfeeding delays were associated with increased mortality after 28 days. The relative risk from 1 to 6 months was similar to the neonatal period for infants with a breastfeeding delay of 1-24 hours, and about half as large for infants with a >24 hour delay.
Comparing EIBF (within 1 hour of birth) to delayed breastfeeding (1-24 hours) under a range of scenarios we think are reasonable (Table 1; spreadsheet with calculations and notes), we estimate that EIBF could reduce mortality by between 7 and 24% in the neonatal period (0-28 days after birth) and between 5% and 17% in the post-neonatal period (28 days to 6 months after birth).
| Time period | Optimistic discount** | Relative risk | Midpoint discount** | Relative risk | Pessimistic discount** | Relative risk |
| 0-2 days | 10% | 0.78 | 45% | 0.86 | 80% | 0.95 |
| 3-28 days | 0% | 0.75 | 30% | 0.83 | 60% | 0.90 |
| 0-28 days* | ---- | 0.76 | ---- | 0.84 | ---- | 0.93 |
| 28 days - 6 month | 30% | 0.83 | 55% | 0.89 | 80% | 0.95 |
* assumes 50% of neonatal mortality from day 0-2 and 50% from day 3-28 ** from unadjusted RR of 1.33 (inverted to present in the form of risk reduction) | ||||||
Table 1. Adjusted relative risks of mortality for EIBF within 1 hour of birth compared to breastfeeding initiation from 1-24 hours.
These estimates are for EIBF, but we think the benefit of immediate SSC is at least as large. EIBF and SSC are closely linked, and we believe the causal direction is primarily from SSC to EIBF (though EIBF could also cause SSC to be maintained for longer). Therefore it is likely that much of the mortality reduction associated with EIBF is actually occurring through pathways linked to SSC.
E. SSC and EIBF have almost no cost and few associated risks
Immediate SSC and EIBF are natural and safe practices requiring nothing more than the newborn and mother. A Cochrane review [17] and a more recent meta-analysis found no experimental evidence of adverse effects of SSC [15].
An extremely rare event that has been reported in association with SSC and EIBF is the sudden unexpected postnatal collapse of an apparently-healthy neonate within the first few hours after birth (which can be fatal or result in neurological injury). This sometimes reflects undiagnosed abnormalities, but in many cases it is attributed to asphyxiation due to airway obstruction with the infant in the prone position (which should be preventable by keeping the nose and mouth visible). The incidence in population‐based studies in Europe ranged from 2.6 to 5 cases per 100,000 births and death rates from 0 to 1.1 deaths per 100,000 live births [43].
Actively promoting SSC and EIBF might induce feelings of guilt or shame in mothers who are unable to practice them, though we did not find studies specifically examining this possibility. Continuing with breastfeeding is also known to have some adverse effects for mothers, such as mastitis (breast inflammation commonly due to infection), nipple and/or breast pain, disrupted sleep, and challenges with employment and other activities. There is also some risk these practices could be perceived as a substitute for full KC programs, which require more resources but have proven benefits (though conversely, it seems very likely that promoting immediate SSC and EIBF would confer some protection to at-risk newborns in contexts where resource constraints prevent full implementation of KC programs).
F. Rates of SSC and EIBF vary widely and are often very low
Reported rates of SSC and EIBF vary substantially between locations, according to all studies and data sources we identified. “Official” rates of EIBF are typically derived from periodic large-scale surveys such as the Multiple Indicators Cluster Survey (“MICS”) or Demographic and Health Survey (“DHS”). In addition, some studies have published rates based on facility medical records or direct observation. Each source has advantages and disadvantages[21].
Reported national rates of EIBF from MICS and/or DHS range from single digits to over 90%, depending on the country. Data are freely available and are incorporated into the “Global Breastfeeding Scorecard”, a project of the WHO and UNICEF. Almost half of the 133 included countries (predominantly low- and middle-income) have EIBF rates below 50%, but 23 countries exceed 70% [44].
The most comprehensive study we identified on the practice of EIBF as documented in medical records examined 373 facilities across 24 countries (predominantly low- and middle-income) [45]. Rates varied from 18% to 98%, averaging 58%, and varied substantially both within and between countries. For SSC, a systematic review examined data from 28 countries, finding inconsistent definitions of SSC and rates between 1% and 98% [46].
Limited data also suggest that SSC and EIBF may be substantially overestimated by survey and medical records. In a study where trained observers recorded breastfeeding timing in five hospitals across three countries, observer-recorded EIBF rates were only 11%, compared to 53% as reported by mothers upon hospital discharge, and 86% according to hospital registers [47]. In another publication on this data set, observed skin-to-skin contact was 42% versus 84% reported on exit surveys [48]. A few qualitative studies among health workers have identified barriers to early SSC [49], [50], [51], including standard hospital routines, questions about staff resources required, and inadequate knowledge, among other factors.
Trends may be context-specific, but we think that overall rates of immediate SSC and EIBF are probably rising in most LMICs. Contributors could include increases in births assisted by skilled attendants [52] and ongoing efforts such as the Baby-Friendly Hospital Initiative (which include promotion of SSC and EIBF) [1].
G. SSC and EIBF can be increased by basic promotional interventions
SSC can be dramatically improved by targeting hospitals and health workers
Several quality improvement interventions using quasi-experimental designs have reported large increases in skin-to-skin contact in hospital-based births, and we did not identify any studies showing null results.
A low-cost health worker training intervention[22] in a Ugandan hospital produced large improvements in the rates of SSC for the first hour after birth [53]. Compared to rates before the intervention, SSC for the first hour increased from 0% to 53% in the three months after the intervention. A qualitative study on the same intervention concluded that “The involvement of health professionals and the observation of the benefits of SSC resulted in a change both in attitudes and in care practices” [49].
Two quality improvement initiatives at tertiary care hospitals in India both showed that it was feasible to achieve vast improvements in SSC for vaginally delivered infants. The first showed an improvement in rates of sustained SSC (over 30 minutes duration) from 0% to 75% over the course of several Plan-Do-Study-Act (PDSA) cycles [54]. The second showed improvements in duration of SSC from 0 minutes at baseline to 67 minutes after intervention, which was fully sustained four years post-intervention [55].
We found fewer studies evaluating EIBF as an outcome (likely because SSC is more directly controlled by hospital practices). A 20-hour training on Baby-Friendly Hospital Initiative practices [1] given to health workers in the maternity unit of a South Sudanese hospital (including doctors, midwives, and nurses) was evaluated in a before-and-after study [56]. EIBF rates improved from 48% before to 91% after training. In women who delivered by caesarian section, EIBF improved from 3% to 60%.
EIBF can be moderately increased by targeting mothers or broader communities
Observational data shows that baseline EIBF rates are positively associated with several factors such as facility-based delivery, SSC, and maintaining visual privacy, and negatively associated with pregnancy complications, birth complications, and cesarean delivery [45], [57], [58].
Experimental interventions designed to promote EIBF among mothers generally appear effective, though the interventions and effectiveness varied substantially in the studies we examined. A 2016 Cochrane review of interventions for promoting the initiation of breastfeeding [59] found only three studies assessing promotional interventions reporting on EIBF. All were delivered by non‐healthcare professionals (counsellors and support groups). The differences did not quite reach statistical significance, though they generally favored the intervention. Three subsequent cluster RCTs found positive results of enhanced breastfeeding education and support programs. The first two were delivered by trained peer supporters. EIBF rates were improved from 77% to 89% in the first [60] and 41% to 73% in the second [61]. A third cluster RCT studied the effects of prenatal education delivered by health workers and found that EIBF rates were higher in the intervention group (73% vs. 60%) [62].
A few community-based interventions have been successful in promoting EIBF. A cluster RCT of an essential newborn care promotion intervention showed improvements in SSC, EIBF, and a large mortality benefit [63]. Cluster RCTs of a large-scale breastfeeding promotion intervention[23] in three countries showed improvements in EIBF rates [64], [65] that were sustained at two-year follow-up [66]. A quasi-experimental pre-post study of a multilevel community and facility intervention promoting immediate SSC and breastfeeding for all babies (both home and facility births) showed improvement in immediate SSC from 8% to 24% and improvement in EIBF from 51% to 68% [67].
The potential “ceiling” is high
SSC and EIBF could be practiced by the vast majority of mothers and newborns. There are few theoretical limits, and observed rates are very high in some countries. The percentage of newborns and/or mothers expected to need emergency medical interventions that would interfere with SSC and EIBF is probably in the single digits [68]. Most standard newborn care procedures (such as ophthalmic ointments) can be safely deferred until after the first hour. Furthermore, routine interventions such as injections and suturing vaginal tears can be performed with the infant in SSC, and SSC may even reduce both maternal and newborn pain during such procedures [69], [70]. It is feasible to achieve substantial SSC and EIBF rates even after cesarean section, and in many settings immediate SSC after cesarean is standard practice.
H. Few actors are working specifically to increase universal SSC and EIBF
When viewed as components of comprehensive newborn care packages, SSC and EIBF receive substantial attention from major global health organizations[24]. Additionally, there are organizations working specifically to promote kangaroo care. While best practice for KC involves immediate SSC, true KC involves longitudinal practices and is specifically applicable to low birthweight and/or preterm infants. The landscape appears considerably more neglected when considering targeted efforts to maximize rates of immediate SSC and EIBF for all newborns. We are unaware of any organizations dedicating resources primarily or exclusively to optimizing these practices or developing context-specific implementation strategies.
Key uncertainties & how we could be wrong
Here we outline some ways our findings could be seriously wrong, in order of what we consider the most likely.
1. Achieving large real-world improvements in SSC and/or EIBF could be more challenging and costly than quality improvement studies seem to suggest. Due to factors including publication bias, observer bias, and the idiosyncrasy and poor generalizability of small-scale initiatives, we think it’s likely that these studies overestimate how much improvement could be expected in a typical case.
2. Targeted intervention may not be truly neglected if “package” interventions are similarly effective and broadly implemented. Some data suggest that training on essential newborn care (which promotes multiple interventions in addition to SSC and EIBF) substantially improves SSC and EIBF rates [63], [71], [72], [73]. If these comprehensive programs are cost-effectively implemented at high scale, this would imply that “stand-alone” promotional strategies may not be necessary, and promotion of these practices may not be as neglected as we suggest.
3. The effects of SSC and/or EIBF could be smaller than even our pessimistic case assumptions. Some specific concerns with the data on EIBF include the observational nature raising possibilities of reverse causation and unmeasured confounders, social desirability bias [74] (particularly that more knowledgeable women might over-report early breastfeeding and also have lower risks for adverse neonatal outcomes), the relatively small number of studies (although they were each large), and publication bias (particularly as all were secondary analyses of cohorts from RCTs on other topics). Our concerns with the experimental evidence on SSC include publication bias (which was often present in the cases where it was assessed in meta-analyses) and a high level of heterogeneity in definitions, interventions, and/or outcomes reported.
4. The effects could also be larger than our optimistic case assumptions. We use the observational evidence for EIBF to help scale the potential benefit of promoting these practices; however, we believe that SSC works through additional pathways which, in combination with the effects of EIBF, could result in benefits beyond the upper range of our estimates. The most optimistic case would also incorporate substantial gains beyond mortality, which we do not attempt to quantify[25].
5. We’re unsure how long improvements from promoting SSC and/or EIBF may last. Some studies reported that their interventions continued to show benefits up to a few years later, but most only included short-term follow-up. In healthcare settings, it seems likely that standard practices may depend greatly on exigencies such as the efficient use of provider time and facility resources. We think that care could be organized to promote SSC and EIBF without demanding extra resources, but we are not entirely certain.
6. We have questions about the reliability of statistics on baseline rates of SSC and EIBF from population-level surveys. In particular, we think that recall bias is likely considering that accurate reporting of these outcomes by mothers after a considerable time (up to two years later) would require a precise and lasting memory of the moments after birth (a time of heightened emotional and physical intensity, which could distort recollections). If baseline rates are higher than surveys suggest, there could be less opportunity for impact. However we think the more likely scenario is that rates are substantially lower than officially reported.
7. The benefits of SSC and EIBF could be largely driven by preterm and/or low birthweight infants. If the overall benefits are largely driven by this subset of infants, promoting universal SSC and EIBF may be less beneficial in areas where KC is being promoted for these high-risk newborns. However, evidence suggests the mortality benefit of EIBF is similar regardless of birthweight [75], and the RCT-established benefits of immediate SSC that we discussed included full-term infants, making it seem implausible that the mortality benefit is unique to low birthweight or preterm infants.
8. The importance of these practices could be changing over time. There has been a substantial decline in neonatal and infant mortality in LMICs in recent years, and much of the evidence we reviewed was generated when mortality rates were substantially higher. We don’t think this should clearly impact the relative benefit of these practices[26], but certain possible mechanisms (such EIBF protecting against consumption of unsafe water in prelacteal feeds) could be less relevant in certain contexts (such as areas where water quality has been improved).
9. We could have missed critical information in our evidence review. Our review process was not systematic. We did not examine every underlying study closely (particularly those reported within meta-analyses). When we dug deeper, our interpretation of the findings often changed slightly. We also did not speak with any subject-matter experts who might have been able to correct our understanding in case we missed or misinterpreted evidence.
Additional research needed
What is the estimated cost-effectiveness of interventions that promote immediate SSC and EIBF among health workers? A preliminary analysis by HealthLearn[27] suggests that its online health worker training, which promotes early SSC and EIBF along with other newborn care practices, is plausibly cost-effective. However, more research (including by independent evaluators) is needed to better understand the costs and likely impacts of different EIBF-promoting programs.
What is the best level for intervention? Immediate SSC and/or EIBF rates seem to respond to interventions among health workers, mothers, and broader communities, but we lack good evidence on comparative effectiveness. There may also be other cost-effective methods, such as mass media campaigns or policy changes to monitor SSC and EIBF among health facility reporting metrics.
Where is the “sweet spot” in terms of cost and effectiveness of promotional interventions for EIBF and SSC among health workers? It seems likely that resource-intensive efforts may improve rates further than “light-touch” interventions. However it isn’t clear whether the optimal cost-effectiveness is found with intensive and costly (but highly effective) interventions or with more basic interventions (which may still have some effect at a much lower cost).
How does the effectiveness and cost of promoting a narrow set of interventions (immediate SSC and EIBF) compare to more comprehensive essential newborn care training interventions? An analysis from GiveWell[28] suggests that such programs are potentially cost-effective, but have “very heterogeneous training content.” It may be that specific components (such as early SSC and EIBF promotion) contribute a substantial portion of the impact of these programs. A better mechanistic understanding of how these programs save lives could increase their consistency and effectiveness.
Can we better calibrate the mortality benefit of immediate SSC by incorporating observational evidence for mortality benefits associated with its other effects beyond EIBF? Our mortality estimates are drawn only from studies on EIBF, but observational studies have also found mortality associations with exclusive breastfeeding, hypoglycemia, body temperature, and cardiac stability.
Disclosures
Vijay Kotecha is an internal medicine physician with over 10 years of experience, including research and clinical work in low-resource settings. He recently completed Ambitious Impact’s Research Training Program.
Marshall Thomas is Executive Director of HealthLearn. He has a decade of experience in online learning, medical education, and global health. He has a PhD in biomedical sciences from Harvard Medical School.
LLMs (Claude and Google Gemini) were used in a limited role for editing this report. They were not used for other purposes such as identification of literature, analysis, or substantive writing.
HealthLearn is an Ambitious Impact-incubated charity that funded this research and played a role in developing this report.
References
- ^
While there is some evidence for KC in full-term neonates, the vast majority of evidence and programs are specific to preterm and/or low birthweight infants.
- ^
- ^
We are unsure why these practices don’t seem to receive more attention, but one possibility is that they may be conflated with related practices such as KC and EBF.
- ^
While immediate SSC and EIBF are closely related, only SSC can truly be manipulated as an experimental intervention. Successful EIBF depends on maternal and newborn behaviors which cannot be directly controlled (although they can be promoted in various ways). Accordingly, SSC has been studied in many randomized trials, whereas the evidence for EIBF is primarily observational.
- ^
Varying by study but including factors such as maternal age, education, wealth, parity, infant birth weight, infant sex, mode of delivery (vaginal or cesarean), location of delivery (health facility or not), and presence of skilled birth attendant.
- ^
Implying that EIBF must involve other mechanisms than simply establishing a pattern of exclusive breastfeeding.
- ^
Discussed further in the section “Key uncertainties & how we could be wrong”
- ^
SSC was categorized as “immediate” if occurring within 10 minutes and “early” if occurring within the first 24 hours.
- ^
Based on meta-analysis of 9 RCTs with 1150 participants, initial breastfeeding success was higher in the SSC group (odds ratio of 2.77). Based on meta-analysis of two studies, breastfeeding duration was longer with SSC.
- ^
Based on five to 13 RCTs including 306-1,369 infants (depending on time point), exclusive breastfeeding rates were higher at hospital discharge, discharge to 3 months, and 3 to 6 months. The gap between SSC and control groups grew over time, ranging from 24% higher at discharge to 146% higher from 3-6 months.
- ^
Based on meta-analysis of six RCTs and one quasi-randomized trial involving 922 infants, study-defined neonatal hypoglycemia was reduced by approximately 70% by immediate SSC.
- ^
For hypothermia, based on meta-analysis of 23 RCTs involving 2,873 infants, study-defined hypothermia occurred half as frequently (relative risk of 0.49) with SSC. For hyperthermia, based on meta-analysis of eight RCTs with 769 infants, study-defined hyperthermia was reduced by around a third (relative risk of 0.67) with SSC.
- ^
Based on meta-analysis of two RCTs, a composite score of heart rate, respiratory status and arterial hemoglobin oxygen saturation in the first 6 hours of life showed greater stability for low-birthweight newborns receiving SSC versus incubator care.
- ^
Based on meta-analysis of 25 RCTs and quasi-experimental prospective trials, immediate SSC moderately reduced the duration from birth to expulsion of the placenta as well as the likelihood of incomplete delivery of the placenta and uterine atony (incomplete contraction after birth), all of which are implicated in postpartum hemorrhage.
- ^
Defined either as feeding a newborn anything prior to the first breastfeeding or as feeding anything other than breastmilk within the first three days.
- ^
Given the strong evidence for benefits, ethically conducted RCTs would not deprive a control group of these practices. Studies could compare standard care versus promotional interventions, but because the control group would have non-zero rates, more participants would be required to detect any differences.
- ^
Supposing that a promotional intervention raised immediate EIBF rates from 30% to 80%, EIBF reduced neonatal mortality by 24% (our most optimistic scenario below), and the baseline neonatal mortality rate was 34 per 1000 (among the highest in the world, https://data.worldbank.org/indicator/SH.DYN.NMRT), a study would require randomizing around 50,000 participants to achieve 80% power (calculated at https://clincalc.com/stats/samplesize.aspx). With less favorable assumptions, the required sample sizes would be even higher.
- ^
Due to systematic ways in which research findings may be generally prone to overestimating effect sizes, as well as some limitations of the evidence on EIBF, we consider those figures as “upper limits” rather than a central point estimates of the true effect.
- ^
Because of how heavily mortality is skewed towards the beginning of life, assumptions about the effects of EIBF in the first few days will have a large impact on our estimate. And although deaths after 28 days are far less common, we also should account for these in an estimate of the total effect of EIBF.
- ^
We take this as weak evidence against reverse causation (where we might expect an enhanced relationship between EIBF and death from day 0-4), though it is theoretically possible that the causal relationship shifts over time without affecting the strength of correlation (i.e., the correlation could begin as poor health resulting in delayed breastfeeding and shift to delayed breastfeeding resulting in poor health, with a similar magnitude throughout).
- ^
MICS and DCS survey data have the advantage of standardization, representative sampling, large numbers, and subnational-level data. However they also have risks of recall and social desirability biases, and exact methods have changed slightly over time (complicating the comparison of trends). In contrast, medical record data and direct observation are less representative (e.g., focused on narrow geographies and excluding home births) but may be more objective.
- ^
The intervention consisted of gaining buy-in from hospital leadership, showing a 1-hour video and delivering a lecture to health workers on the benefits of SSC and breastfeeding, conducting focus groups and interviews among staff to identify opportunities and barriers, distributing pamphlets, hanging posters in delivery rooms, and distributing “SSC ambassador cards” to staff who completed interviews.
- ^
“Alive & Thrive”, involving interpersonal counseling plus mass media, community, and policy components.
- ^
For example, the WHO's Essential Newborn Care course, UNICEF's Every Newborn Action Plan, and Save the Children's Saving Newborn Lives program all incorporate SSC and EIBF as elements within broader maternal-newborn health frameworks.
- ^
For example, EIBF promotes EBF, and EBF is associated with many benefits including fewer childhood infections, higher intelligence, lower rates of metabolic disorders, and reduced rates of breast and ovarian cancer in mothers.
- ^
Though it does mean that a lower absolute number of neonatal deaths would be averted now compared to when the studies were conducted, assuming the same relative reduction.
- ^
- ^

Also of interest on this topic: Ansh, a CE-incubated charity on kangaroo care for newborns.
I made a tag for posts about maternal and newborn health.
Excuse my ignorance & offtopicness, my knowledge here is moderate reading of Oster-like books & Rationalish blogposts & the like aimed at UMC parents, and being present for the birth of my kids in NZ's midwife-led maternity system.
What is the alternative to immediate skin to skin contact? Is this is "medical professional takes kid away to measure & do heel prick etc. while someone else looks after mum" situation? Is this in a cultural context of total deference to medical authorities or how on earth does this become normalised? What is common in the US? (looks like immediate SSC is also the US standard: https://www.reddit.com/r/BabyBumps/comments/1dmarxj/how_do_i_make_sure_to_get_skintoskin_with_my_baby/)
It's wild to me that this isn't already the standard, I can't imagine what they're doing instead.
There's no heel prick in low income countries because there isn't the money for newborn screening.
Yep here it's super common here in UgAnda the baby gets whisked away to check breathing, temperature, then gets washed, then gets wrapped up. Often babies are then given to mother wrapped in clothes. Skin to skin is highly variable and I would say the majority of babies don't get it.
We should be careful about criticizing cultural norms. Cleaning and wrapping up the baby is often seen here as the best care they can get - it's just unfortunate that it isn't.
I don't think it's that wild that it isn't the standard, I can easily see how other options after birth could be seen as "better" for a whole bunch of reasons.
Agree - in general when we want to keep someone warm we wrap them in warm clothes or blankets. I can see why it's not intuitive to keep the baby undressed (and keep them warm in a different way).