
This summer, I participated in a human challenge trial at the University of Maryland. I spent the days just prior to my 30th birthday sick with shigellosis.
What? Why?
Dysentery is an acute disease in which pathogens attack the intestine. It is most often caused by the bacteria Shigella. It spreads via the fecal-oral route. It requires an astonishingly low number of pathogens to make a person sick – so it spreads quickly, especially in bad hygienic conditions or anywhere water can get tainted with feces.
It kills about 70,000 people a year, 30,000 of whom are children under the age of 5. Almost all of these cases and deaths are among very poor people.
The primary mechanism by which dysentery kills people is dehydration. The person loses fluids to diarrhea and for whatever reason (lack of knowledge, energy, water, etc) cannot regain them sufficiently. Shigella bacteria are increasingly resistant to antibiotics. A disease easily treatable by lots of fluids and antibiotics is becoming more lethal.
Can someone do something?
The deal with human challenge trials
Clinical trials in general are expensive to run but pretty common; clinical trials where you are given the disease – “challenged”, AKA “human challenge trials” – are very rare. The regular way to investigate a possible treatment is to make a study plan, then find people who have the disease and offer to enroll them in the experimental treatment. Challenge trials are less common, but often more valuable for research – shigellosis is a fast-acting disease that is imminently treatable by antibiotics and uncommon in the US. It would be very difficult to test an alternative shigellosis treatment in the US in the conventional way, but it’s a great candidate for challenge trials.
I’d signed up for email alerts on upcoming challenge trials at the nearby University of Maryland, and got one about an upcoming study. It caught my eye that it was for a phage-based treatment. Bacteriophages are really promising antibacterial medicines, not to mention what I’d studied as an undergrad.
Here’s the thing: you really only get good medical research out of human subjects. Also, I could use $4000 and this seemed like a cool way to spend a couple weeks and help out medical research. So I signed up, got a check-in general health appointment, and shortly after, was told I was in. I made plans to spend my 30th birthday in a dysentery ward.
Dysentery: it’s a modern disease
Many of you reading this will know about dysentery from the 1971 simulation game The Oregon Trail (or its later versions). The actual Oregon Trail was a network of trails and the corresponding migration of mostly-white pioneers, moving on foot and on ox-drawn wagon from the eastern US to the western US between 1830 and 1869. About 400,000 people* crossed the Oregon Trail in this period, and a lot of them were on similar trails – a bunch of stressed and malnourished people, traveling in close quarters with their families, stopping and pooping near the same trails and creeks with no regard for water safety – diseases spread very fast in these conditions. From these and other stressors, about 65,000 people died in this 40-year period.
Stated another way, more people die from dysentery now, every year than ever died from any cause on the Oregon Trail. So let’s calm down about the Oregon Trail, okay?
*Lots of people use this 400,000 number but I can’t figure out where it came from and if this is referring to individuals or families – I’ve seen sources indicate it was either. If it was families, it was probably counting the men who were “the pioneers” and then being like “oh and there were women and kids there also, I guess.” But maybe it was individuals? Or maybe someone just made this up? Again, no idea where it came from. You gotta be careful every time anyone tells you a number. It’s so bad out there. The only thing worse than someone telling you a number is when they don’t tell you a number.
Getting ready
A week or so before I went, I’d been pointed to Jake Eberts’s twitter thread. Jake Eberts also participated in a challenge trial for a dysentery vaccine, also I think at UMD and the same Baltimore facility I was at, where he got very sick and went viral for livetweeting the experience. He started a fundraiser for dysentery relief and got a lot of people to sign up for clinical trials themselves, and now he works for 1DaySooner, premier “hey, human challenge trials are cool” advocates.
I read his twitter thread and sent my friends this meme:
I brought Infinite Jest, which I was partway through and was a lot more through (but still not done) by the time I was discharged. (I’m writing this while traveling, and in a fit of poor timing I finally finished it on the plane ride in, which means I now have a giant brick of a book to carry around in my suitcase.) My friend Ozy said that Infinite Jest was a really good book for reading in a dysentery ward.
I thought, oh, that’s interesting, you know, a lot of the characters are pretty miserable and living in a controlling institution of some kind. Then I remembered this one passage, where circumstances have forced a character into withdrawing from heroin alone, holed up for days in a public bathroom:
Time began to pass with sharp edges. Its passage in the dark or dim-lit stall was like time being carried by a procession of ants, a gleaming red martial column of those militaristic red Southern-U.S. ants that build hideous tall boiling hills, and each vile gleaming ant wanted a minuscule little portion of Poor Tony’s flesh in compensation as it helped bear time slowly forward down the corridor of true Withdrawal. By the second week in the stall time itself seemed the corridor, lightless at either end. After more time time then ceased to move to be moved or be move-throughable and assumed a shape above and apart, a huge, must-feathered, orange-eyed wingless fowl hunched incontinent atop the stall, with a kind of watchful but deeply uncaring personality that didn’t seem keen on Poor Tony Krause as a person at all, or to wish him well. Not one little bit. It spoke to him from atop the stall, the same things, over and over. They were unrepeatable. Nothing in even Poor Tony’s grim life-experience prepared him for the experience of time with a shape and an odor, squatting; and the worsening physical symptoms were a spree at Bonwit’s compared to time’s black assurances that the symptoms were merely hints, signposts pointing up at a larger, far more dire set of Withdrawal phenomena that hung just overhead by a string that unraveled steadily with the passage of time. It would not keep still and would not end; it changed shape and smell.
I was forced to agree that Infinite Jest was indeed probably a pretty good choice.
Two days until challenge
Checking in, everyone’s bags were checked. I got the impression they really didn’t want some kind of bad outcome where they had to call cops into a ward where everyone was running around with the bloody flux, which, fair enough. They did take away my craft scissors. I didn’t end up knitting so it wasn’t a big deal but like I’m pretty sure I’ve taken those on airplanes before. Okay.
We were assigned a number (I was just on this side of divinity at No. 107), given a plastic wristband, and shown to our rooms. We were also given two pairs of scrubs which were to be our main clothes on the ward – less risk of ruining hard-to-launder clothes in the more messy phases of the study – though it did mean 15 people having to coordinate laundry every day.

The ward was more of a retrofitted office building than a hospital. It consisted of some spaces for nurses and testing, about 6 bedrooms of various sizes (each with their own half-bath), two separate areas with two shower stalls each, a “kitchen” with snacks and where the meals were delivered to, a closet with washer and dryer, and a rec room with couches and a TV and a pool and foosball table.
There were about 16 people on the ward, an even mix of men and women. Most of them were Baltimore locals; many of them had done other trials before. We were fully allowed to socialize – dysentery is, again, infectious through the fecal-oral route, hand sanitizer was stationed all over the place but there wasn’t a huge concern that we’d infect each other or even the nurses.
Life on the ward is very chill. I was worried about being bored, but I’d forgotten that I spend most of my waking hours on the computer anyway, so it really wasn’t a problem. When even my iron gaze faltered and couldn’t stare at the computer anymore, I read Infinite Jest.
Meals were delivered once a day – one cold usually wrap- or sandwich-based meal, one hot breakfast, one hot supper dish, labelled with people’s numbers.

They were, like, fine. The caterers made a few interesting choices – for vegetarians such as myself, every sandwich/wrap was some veggies with hummus, and now and then there’d be like breakfast pancakes with a curry-flavored veggie hamburger patty. I would describe the flavor when drenched with table syrup as “weird.”
Like, you can tell the person planning that menu was like “okay, pancakes and bacon… And wait, crap, something with protein for the vegetarians.” But again, I’ve eaten worse for things I’ve actually paid for ingredients for, and I was definitely eating better in terms of variety and volume than I did at home. I’m not complaining.
One day before challenge: the age of phage
This study was sort of an over-time test – ideally the first of a few, where we’d get phages before (unless we were in the control group), during, and after the “challenge” (the shigella) to see if they had any effect at all – if it did, later studies could determine if you could just drink the phage after getting sick, or if it would work best as a prophylactic, or etc. We drank a chalky buffer solution to neutralize stomach acid and give the bacteriophages (and later, the bacteria) a better chance at making it to the intestine.
What do the solutions taste like? Basically all salty fluid with slight mineral nuance, from the buffer. Phages are known to be pretty tasteless so I didn’t expect anything else.
Bacteriophage therapy: sending a cat after mice
A bacteriophage is a virus that infects bacteria. They were discovered shortly after bacteria themselves were really pinned down – microscopes were finally powerful enough to make out bacteria, and visionaries like Robert Koch and Louis Pasteur were pinpointing that these little nothing-pinpricks were in fact the source of diseases. (For more on the discovery of the microbial world, see “Through the Looking Glass and what Zheludev Et Al. (2024) Found There”, my recent piece in Asterisk Magazine.)
In 1917, Félix d’Hérelle found an agent that killed cholera bacteria, which passed through a fine filter, and which could reproduce – a living agent that killed bacteria, but that was itself smaller than a bacteria.
d’Hérelle realized right away this substance which killed bacteria, and which people had apparently been drinking, had potential as medicine. He bred pathogenic bacteria in vats and added solutions, and waited until the cloudy brother of bacteria turned clear – then offered this liquid to sick patients. Many of them, sure enough, recovered. I was (unless I was in the control group) walking in historical footsteps. Dysentery was the first human disease ever treated with phage medicine.
Sending a phage after bacteria is like sending a cat after mice. Phages are small, targeted, well-adapted hunters of specific bacteria. There is no way for them to infect a human cell like a human virus would – they are completely specialized. Phages are already in the body, along with their bacterial hosts – so you’re not introducing a radically new agent – and the immune system tends to play well with them.
Phage are used widely in some parts of the world – the Republic of Georgia and Poland both sell phage over-the-counter, for use in say intestinal conditions or wounds, and have clinics for personalized treatment. In the US, phage therapy is an extremely rare specialty, sometimes even falling under the umbrella of naturopathy. (A phage being a natural bioactive product.)
Why would you use antibiotics instead of phages, or vice versa?
| Phages | Antibiotics |
| Targeted – a phage attacks one species or one strain of bacteria Easy to find usable new ones More finnicky (e.g. less stable) Predator-prey pharmacokinetics Mostly spread where the bacteria are Very few side effects | Broad-spectrum Hard to find usable new ones Shelf stable Regular blood-elimination-curve pharmacokinetics Systemic; enter the bloodstream Sometimes-serious side effects |
What if the bacteria become resistant to the phages too?
Well, that can happen easily – probably even easier than with antibiotics. Cells have been duking it out with viruses since the beginning of life. (Did you know CRISPR-Cas9, now used for gene editing, evolved in nature as a way for bacteria to recognize and cut up phage DNA?)
But the difference is that whereas new antibiotics are very hard to find, there is a nigh-inexhaustible evolutionary font of phages constantly pulling ahead in the arms race. So in short: once a bacteria becomes resistant to your special phage, just find a new phage.
Do they work?
To my knowledge, there aren’t any really gold-standard reviews comparing phages head-on to antibiotics. They are fiddlier than antibiotics, with a specialized body of knowledge for treatment – less stable, have to be introduced to the site directly, much more care in choosing an appropriate treatment.
One small study found a phage treatment comparably effective to antibiotics for Salmonella typhimirium in 36 lab mice.[1] Another meta-study compared modern antibiotic studies to 17 studies from the last time human phage research was in vogue in the US, the 1920s-40s, and found that phages were effective treatments – but 4 modern clinical trials suggested phages were not effective.[2] A more recent study of personalized phage therapy showed promising results in infections considered “difficult-to-treat”.[3] They seem to work best when used with antibiotics.
I’m not doing a full lit review right now. I bet that phage therapy still has promise – more careful formulations and just more research will help. That’s before challenges of commercial rollout, including things like handling FDA approval for a product that must be reformulated regularly.
The elephant in the room is antibiotic resistance – antibiotics usually work extremely well, but increasingly, bacteria can survive them. Antibiotic resistance is, unlike other diseases you might think of that are exacerbated by over-medication, not a condition of privileged countries – lots of Shigella bacteria in developing countries are increasingly antibiotic-resistant.
Even if phages don’t work as well as the magic silver bullet that is antibiotics, they might work well enough to be worth incorporating into our medical toolbox as part of AMR management. And that means developing them now.
The other challenge is of course regulatory – I’m excited that Intralytix, who made the experimental product I did-or-didn’t take, is throwing their hat into the space of human phage medicine, and to see how they handle this.
Day 1 of challenge
On the third day in the ward after a day of baseline and a day of phage (unless we were in the control group), we took another dose of phage (unless we were in the control group), waited a couple of hours, and then drank a glass of shigella. This tasted like baking soda and salt with no particular nuance, nor would I expect nuance; the dose was some 1300 organisms – as in 1300 individual cells of bacteria, count ‘em. A preposterously scant microbial innoculum, even for devoted parasites it often takes on the order of millions of organisms to lodge an infection – but shigella is remarkably tenacious. It would only have taken 10-200. This was overkill – a dose that WILL make you sick, unless you’re protected. All the participants drank.
The waiting game
Shigella has a 24-72 hour incubation period, maybe 12-96 hours on the far ends.
Perhaps owing to quirks of my own psyche, whose origins I’m sure we don’t need to explore here, I find it reassuring to have reference experiences to conveniently benchmark the rest of my life by. If you go skiing, you can ask yourself later, “is this more or less exhilarating than skiing?” If you fall in love once, you can compare future loves to that earlier experience.
A good standard reference point for “shared, resigned dread” is the 72 or so hours in a clinical trial ward after everyone has ingested shigella bacteria along with maybe-a-treatment.
The vibes were ominous. Jovially nervous. Unprecedented gastrointestinal distress may or may not have been coming for me, but if it is, it would be arriving in (on average) 48 hours.
The floor was pretty quiet. The hours ticked by.
Infinite Jest is, by the way, a great book. David Foster Wallace knew how to write a goddamn sentence on purpose.
Let’s learn about Shigella pathogenesis
While I waited, I decided to read up. Shigella bacteria invades the body via the digestive canal, and infects the intestines – both small and large. It releases a toxin that facilitates its infection of other parts of the intestine and its eventual replication. It’s an intracellular pathogen – some bacteria, like all viruses, actually enter the host’s cell and replicate inside there.
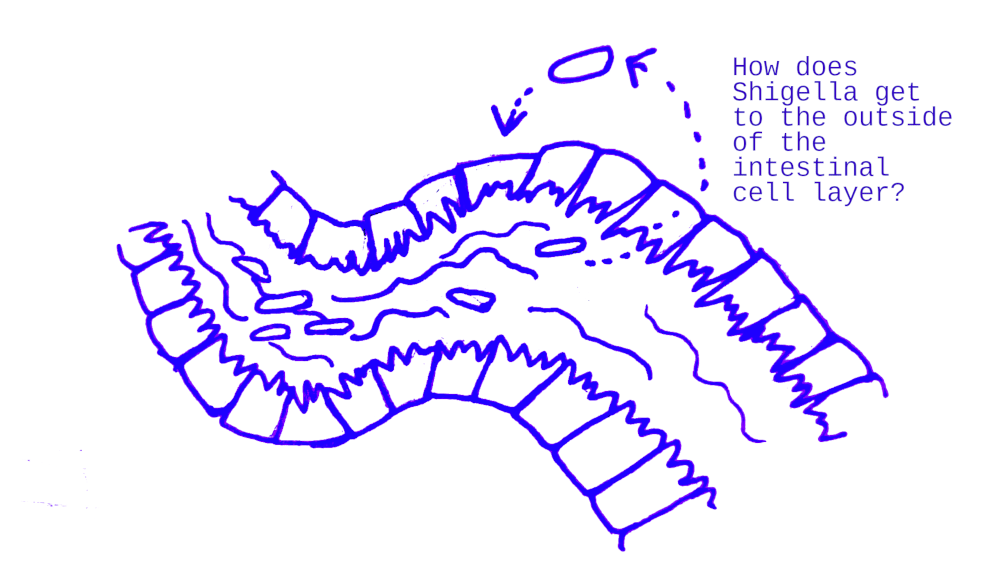
Shigella actually prefers to invade the outside (or should I say the inside?) of intestinal cells. But the body is a locked-down system with its own guard force, the immune system, keeping the dirty external environment separate from the sterile inside environment. Shigella in the digestive tract really wants to poke through that line of intestinal cells and get at them from the other side.
Once inside of the colon, S. flexneri can penetrate the epithelium in three ways:
1) The bacterium can alter the tight junctions between the epithelial cells, allowing it to cross into the sub-mucosa.
2) It can penetrate the highly endocytic M cells that are dispersed in the epithelial layer and cross into the sub-mucosa.
3) After reaching the sub-mucosa, the bacteria can be phagocytosed by macrophages and induce apoptosis, cell death. This releases cytokines that recruit polymorphonuclear cells (PMN) to the sub-mucosa. S. flexneri still in the lumen of the colon traverse the epithelial lining as the PMNs cross into the infected area. The influx of PMN cells across the epithelial layer in response to Shigella disrupts the integrity of the epithelium allowing lumenal bacteria to cross into the sub-mucosa in an M-cell independent mechanism.
This is really funny. Okay, imagine there’s a blockade of tightly parked police cars facing you and you and your buddies need to go get to their trunks so you can hide in them. Here are 3 ways to do this:
- Push the police cars to the side so you can walk between them
- Look for the police cars with the biggest doors, so that you can squeeze through the car and leave through their trunk (or I guess probably just stay in the trunk at that point)
- Get yourself and your buddies arrested, then when they send backup police vans to push through the police to arrest all of you, run through the cracks in the blockade that those vans open up. Then go to the trunks of the original cop cars.
And then once you’re inside the car, you can open the doors between the cop cars (they’re sliding doors) and then travel laterally between the cop cars. I love cells.
As a fun side note, Shigella – including the strain I was developing an intimate relationship with, Shigella flexneri – is, taxonomically speaking, a kind of Escherichia coli. Now you may notice from the scientific nomenclature that this is not how this is supposed to work.
When genotyping was developed and applied to some familiar standby kinds of bacteria that microbiology-as-science figured it understood pretty well, researchers learned two surprising new things:
- E. coli is not a coherent species. Different strains of E. coli – known to have slightly different properties, but thought to be all slight variations on the same basic species – turned out to have only 20% of their genes in common. (Humans and our closest relatives, chimpanzees, have almost all of our genes in common* and still aren’t considered as the same genus.)
- Shigella is in that umbrella of shared genes – a secret family member known as a taxon in disguise. It’s more similar to many E. colis than some E. colis.
For most species, the procedure at this point would be to throw in the towel and reclassify – Escherichia coli spp. shigella, perhaps. But in this case, shigatoxin-producing Shigella and other pathogenic Escherichia coli have different enough clinical presentations that the distinction is still medically valuable, so accurate nomenclature has bowed its head to practicality. Cool! (Compare and contrast with trees.)
*Wait, don’t people talk about 99% or something? That number is actually about sequence similarity and not related genes – if we have 96% sequence similarity, meaning the exact same genetic code, probably even more of that genome is still in related genes. Genes can code for clearly related proteins/sequences and still not be identical, like they came from a common ancestor and haven’t diverged much but have picked up a few changes along the way. Different E. coli have 80% completely different genes – a human has maaaybe 50 genes that a chimp doesn’t? I didn’t try very hard to find the actual similar metric between them. It’s what I was telling you about numbers. You gotta watch out.
Let’s really learn about Shigella pathogenesis
Some 24 hours in, the first people started going down. Via word of mouth I heard the phrase “Exorcist-style projectile vomiting” used to describe someone in the next room over, a description whose accuracy I fortunately cannot verify. Most people were in their rooms all day anyhow, but the crowd in the kitchen at mealtimes or showing up for morning dosing got thinner.
I really held out. Going to bed at end of the second night, I felt okay, but couldn’t sleep well – nerves, I thought, or the faint distorted unpleasant bodily noises from other parts of the ward. I maybe managed a couple hours of sleep by the wee hours.
48 hours in, I woke up for vitals and dosing at 6 AM and started feeling really faint on the short walk to the next room. I stumbled over to the toilet. Off to the races!
I should be clear in this section that I was in as close to zero long-term danger as you can get with dysentery, which is damn close – this was in a controlled setting with doctors and nurses, monitoring my condition regularly, with a known pathogen with a known cure. In this case, we weren’t expected to languish in indefinite misery – they wanted to see if we got sick and then how sick we got, yes, but only up to a point, at which point they would “call it” – administer regular antibiotics and end our experimental treatment.
All I had to do was let the time pass.
The next few hours were very bad. Surprisingly, the gastrointestinal symptoms were not much of a problem for me – I had them, but it wasn’t much worse than those of regular food poisoning. I didn’t throw up. I just wanted to go back to sleep.
But sleep wasn’t coming.
First was the plague of chills. The institutional cotton blankets did nothing; four of them also did nothing, as if there was no heat to hold in. Freezing, tooth-clattering cold.
Within an hour came the plague of joint pain. It sank in rather quickly and was all in the lower extremities – hips, legs. Any more than one blanket became too heavy to bear having on them, so off they go, freezing cold but they weren’t palpably doing anything anyway. Right? I remembered reading people with chronic pain reporting that sometimes laying down was worse than other positions, and sure enough sitting up was – somehow – mildly better. I situated the adjustable bedside table so that I could slump onto it and maybe even sleep like that, but sleep remained out of reach.
Time wasn’t shitting so much as dragging, by the bones, over rough pavement, every second another six inches, grating, relentless, second after second after second. Time is space in which you are moved forward one way or another. Pain is an active process.
Around three hours later, the doctor came in and judged that I was done – they were calling it – symptomatically I had reached the Clinical Endpoint and would be treated. I was handed tylenol and antibiotics.
I’d always thought of tylenol as sort of a second-rate painkiller, probably worth trying if you couldn’t find ibuprofen, but damn if that tylenol didn’t work pretty quickly. As soon as I could I went to sleep for like four hours – which, as usual, if you are in a position of needing four hours of sleep, makes a lot of things better and more manageable once you can swing it.
Out the other side
The antibiotics worked really quickly. Within hours, the fever had vanished and the aches had dwindled to twinges. Within a couple days, even the gastrointestinal situation was back to normal. Other people were harder hit, other people were just starting to get sick – staying vanished in their rooms even after I stuck my head into the kitchen and rec rooms like the first hopeful groundhog of spring – and many had been fine the whole time.
The thing that kills people in dysentery is dehydration and complications thereof. So part of the recovery is collecting and measuring how many fluids were emitted, and then re-administering oral rehydration fluid – a salty liquid served ice-cold – in precise ratios to replace the bodily fluids lost. A human is a series of tubes with attached nervous system and fortunately I was in the company of master plumbers. Once the diarrhea had stopped, I was also able to stop guzzling big plastic cups of what I liked to imagine tasted like arctic seawater. Progress!

People who recovered and who never got sick started hanging out in the rec room more, chatting and playing pool. I spent my birthday calling my parents and talking to internet friends. One streamed himself playing a fish-themed video game in my honor. The Baltimoreans inexplicably set off fireworks many nights – maybe the proximity to July 4th? – and this was one of them. Not roadside-stand-ground fireworks, but big aerial fireworks. A fellow subject found ice cream bars in the kitchen freezer and kindly brought me one as a present. Fireworks aside, it was a quiet day.
Apologies for the deception, reader. Technically speaking, the word “dysentery” usually refers to a syndrome, like “psychosis” or “high blood pressure”, which can have multiple causes but which is defined by specific symptoms. The specific symptom of dysentery is bloody diarrhea. I personally did not get this particular symptom – I became sick with shigellosis but, according to a common criteria, did not get dysentery. I’m sorry for clickbaiting you. In my defense, I would have taken it over the joint pain.
Aftermath
Twice a day after antibiotics, we gave the nurses a stool sample – these were sampled and cultured at some lab to determine if shigella was still in there. Two negative samples in a row meant that we were free to go.
9 days after coming in, I was cleared for release. I collected my scissors, and, free of dysentery, was released onto the streets of Baltimore. A year older on paper. Healthy, wrung out, ready for time to keep doing what it does. Hopefully, mostly on kinder terms.

I think that despite my relatively mild case, that I was in the control group. But the reason I think that was because in the whole trial, everyone drank the shigella, and it sure seemed like about half of them didn’t get sick at all.
Pretty goddamn cool, if you ask me.
If you want to have study rigor performed on your body, you can look for clinical trials at clinicaltrials.gov. 1DaySooner advocates for human challenge trials; they have a list of challenge trials that are actively recruiting and you can also sign up for email alerts. Many of them pay money. Consider checking it out.
Thank you Grace Neptune, Kelardry, and YumAntimatter for reviewing a draft of this post.
I have a Patreon! Consider supporting my writing by throwing me a few bucks. I’d really appreciate it. I won’t be getting dysentery again (…on purpose) but I have some other good stuff in the works.
Posted on [Eukaryote Writes Blog - Substack - Lesswrong - EA Forum]
- ^
R. a. N. Acebes et al., “Comparing the Efficacy of Bacteriophages and Antibiotics in Treating Salmonella Enteric Serovar Typhimurium on Streptomycin-Pretreated Mice,” Philippine Journal of Science (Philippines) 150, no. 6a (2021), https://agris.fao.org/search/en/providers/122430/records/6474afaca3fd11e430380e4f.
- ^
Luigi Marongiu et al., “Reassessment of Historical Clinical Trials Supports the Effectiveness of Phage Therapy,” Clinical Microbiology Reviews 35, no. 4 (September 7, 2022): e00062, https://doi.org/10.1128/cmr.00062-22.
- ^
Jean-Paul Pirnay et al., “Personalized Bacteriophage Therapy Outcomes for 100 Consecutive Cases: A Multicentre, Multinational, Retrospective Observational Study,” Nature Microbiology 9, no. 6 (June 2024): 1434–53, https://doi.org/10.1038/s41564-024-01705-x.


Very impressive - I don't think I have the stomach (so to speak) to put myself through this kind of suffering. Thanks for doing something so selfless and unpleasant for the benefit of anonymous others ❤️
Kudos for doing this. I attribute my ongoing IBS to a case of dysentery caught in the wild, hope you don't suffer similarly!
Executive summary: The author voluntarily participated in a human challenge trial for dysentery, experiencing the disease firsthand to contribute to medical research on bacteriophage treatments and raise awareness about a deadly global health issue.
Key points:
This comment was auto-generated by the EA Forum Team. Feel free to point out issues with this summary by replying to the comment, and contact us if you have feedback.