Authors: Kaitlyn Hobbs, Sophia Seidler, Mo Putera
Reviewer: Morgan Fairless
Date of publication: December 2023
Research period: Research Training Program 2023
This report was conducted within the pilot for Charity Entrepreneurship’s Research Training Program in the fall of 2023 and took around eighty hours to complete (roughly translating into two weeks of work). Please interpret the confidence of the conclusions of this report with those points in mind.
Thanks to Morgan Fairless for his contributions to this report. We are also grateful to the experts who took the time to offer their thoughts on this research.
For questions about the structure of the report, please reach out to leonie@charityentrepreneurship.com. For questions about the content of this research, please contact Mo Putera at mputera1@gmail.com, Sophia Seidler at sophiaseidler1@gmail.com, or Kaitlyn Hobbs at kaitlynjhobbs@gmail.com.
Executive summary
This report aims to outline our research on implementing an intervention that provides palliative care, including pain medication (e.g., opioids), to individuals experiencing severe health-related suffering (SHS) due to a life-threatening disease.
Each year an estimated 20 million people are in need of palliative care in the last year of their life, with many more requiring palliative care prior to the last year of their life. Of these people in need, 78% live in low- and middle-income countries. For children, 98% of those needing palliative care live in low- to middle-income countries with almost half of them living in Africa. In 2014, it was estimated that only 14% of people needing palliative care at the end of life, actually receive it.
Globally, Sub-Saharan Africa (SSA) is referenced as one of the most under-developed and under-serviced region when it comes to awareness and provision of end-of-life care. Palliative care is an essential component of medical care for incurable, life-threatening illnesses to reduce the suffering of those affected.
We propose enhancing palliative care accessibility by providing medical advice, safe access to pain management, and additional support as necessary, collaborating with existing hospitals and community health centers to identify and systematically address gaps, offering training to local staff, and supplying required materials and medications to facilitate palliative care both at home and in hospital settings.
To ameliorate the burden of suffering in SSA, we propose implementing a charity that trains staff to deliver at-home palliative care.
We found evidence to support the idea that a charity could make change in this space, as exemplified by Hospice Africa, but did not find any studies or impact assessments that evaluate the effectiveness of current organizations.
We evaluated candidate countries in SSA for increased or improved PC services based on the scale of suffering burden as well as indicators of neglectedness and tractability. That said, several caveats should be kept in mind when interpreting the results. All in all, these factors proposed Zimbabwe as the top candidate region.
We confronted challenges in evaluating an outcome during our cost-effectiveness analysis but ultimately resolved this by reporting the cost per day of serious-health suffering (SHS) averted. With discounting, the geometric mean of the analysis came to $5.35 per SHS day averted.
Altogether, we propose funding a pilot project with a monitoring & evaluation component to fill the evidence gap for effectiveness.
1 Background
1.1 Definitions and scope
1.1.1 Defining palliative care
Palliative care is considered specialized medical care focused on providing relief from the symptoms and stress of a life-threatening disease. The goal is to improve quality of life for both the patient and the family. It is applicable at any stage of a serious illness and can be provided alongside curative treatments. The care team often includes doctors, nurses, and other specialists who work together to provide an extra layer of support aiming to address as many needs as possible including not only physical but psychological, social and spiritual needs.
It is proposed that palliative care needs slightly vary in the context of Africa compared to generalized global definitions (Clark et al, 2007). In addition to pain and symptom management as well as emotional, social, and spiritual support, income generation and financial support for food, shelter, and funeral costs, among other needs, may be included in palliative care in Africa. That said, our theory of change outlined in this report only details provision of physical and psychological pain management tools but has the capacity to develop social, spiritual, and alternative means of pain relief in collaboration with local entities after a formal needs assessment takes place (see 3.4 Approaches to Evaluation).
1.1.2 Models of Palliative Care Delivery in Sub-Saharan Africa
An observational study of palliative care in Kenya and Malawi in 2015 generalized three models of provision of care (Clark et al, 2007): The specialist service model, district hospital model, and community model. The specialist service model entailed provision of care, referrals, and knowledge-sharing typically led by a doctor. District hospital models were often nurse-led and provided the most diverse range of services including but not limited to bereavement, social and nutritional support. Care was provided to in-patient, out-patient, and home-based patients and referrals for continued care could be made to other hospitals, health centers, or specialist clinics. The community model was also typically nurse-led but differed from the prior two models in that it would not be able to refer patients for continued care elsewhere. Care provision was holistic but relied on volunteers.
1.1.3 Benefits of providing at-home palliative care
- Increased access to care for those not living near a hospice or hospital or where capacities are reached
- Avoids capacity limitations and cost of hospital transfers for in-patient care
- Allows individuals to die at home, as preferred
- Generally cost-effective, according to WHO’s programme guide and Lancet Commission
Due to the aforementioned benefits of providing at-home kits and PC services over in-patient care, the former became the focus for the proposed theory of change.
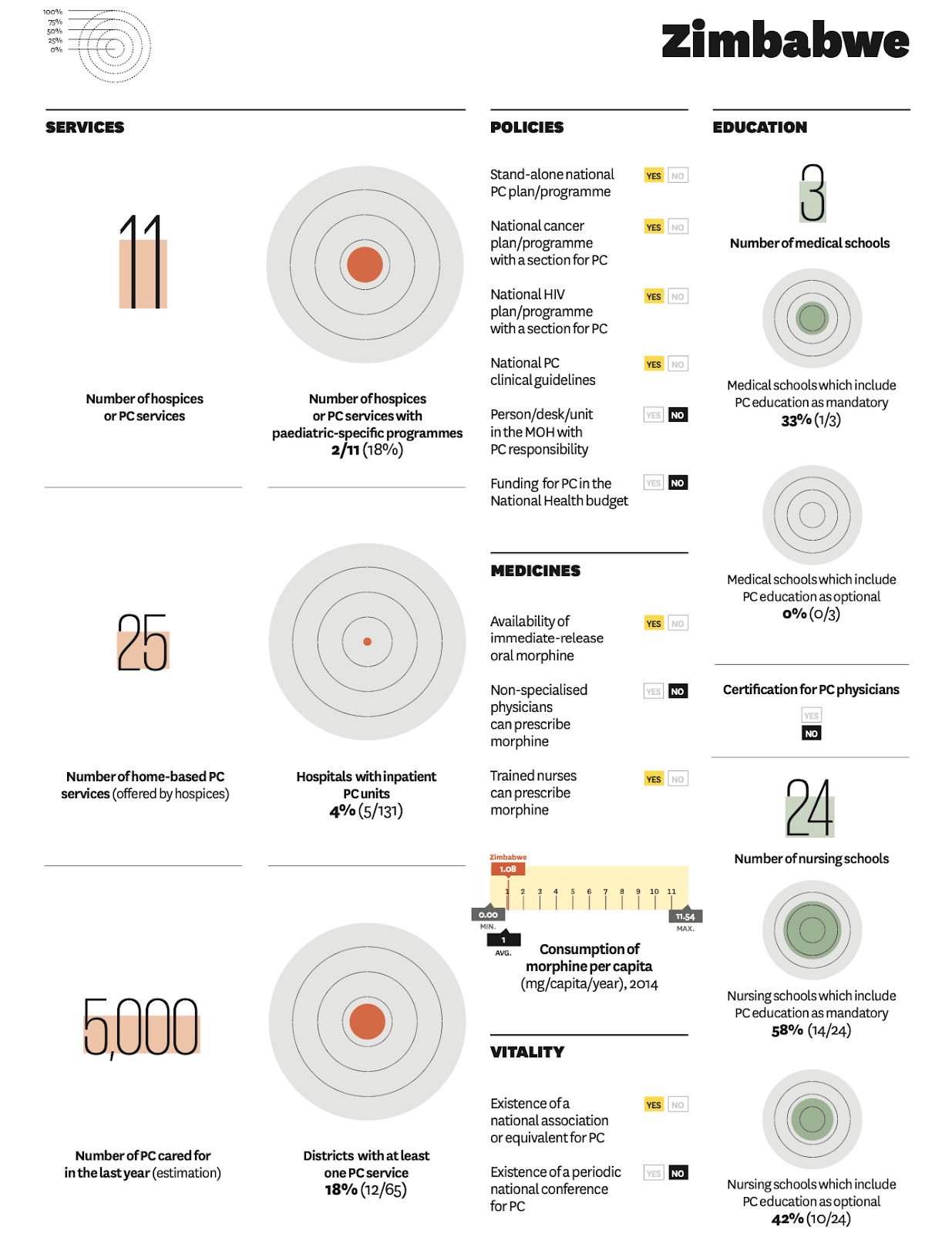
1.2 Order of magnitude of the problem addressed
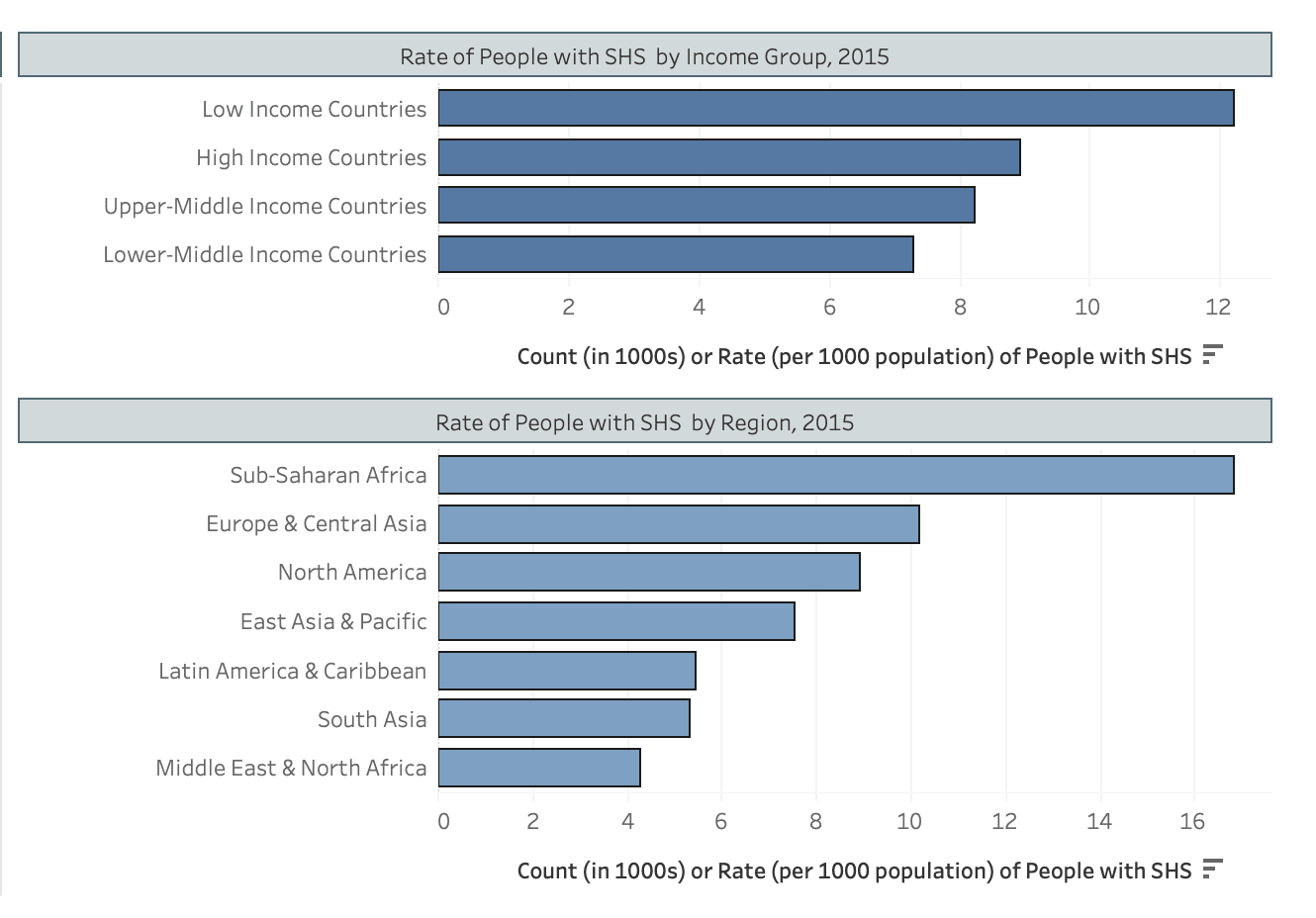
Serious health-related suffering (SHS), defined by Lancet Commission as suffering that cannot be relieved without medical intervention and when regular functioning is compromised (Knaul et al, 2017). SHS is often experienced by individuals at end-of-life. Around 78% of people in need of palliative care in their last year of life live in LMICs with only 14% of them receiving it (World Health Organization, 2016; Connor et al, 2020). Nearly half the number of children in need of palliative care in LMICs live in Africa. The figure below highlights the global burden of serious health-related suffering (SHS) where, within LICs, Sub-Saharan Africa (SSA) carries the greatest share (International Association of Hospice and Palliative Care, 2015). Given several reports and data sources indicating a large burden of end-of-life patients in Africa, we decided to focus subsequent research there.
Figure 1. Rate of people per 1,000 population with SHS by income group (top) and region (bottom).
1.2.1 Importance of Palliative Care
WHO’s Global Atlas of Palliative Care states that the accessibility of palliative care is an obligation under international human rights law as the right to palliative care and pain relief is recognized under the human right to health.
1.3 Cause area review
Previously, Happier Lives Institute (HLI) conducted a cause-area review for pain relief in which increasing access to opioids in palliative care of LMICs was estimated to be most promising (Dupret et al, 2023). In decreasing order of estimated cost-effectiveness, other evaluated intervention strategies included: supplying palliative care centres with opioids in LICs, increasing access for migraine medication in LMICs, and task-shifting psychotherapy for chronic pain.
A previous investigation into pain relief in low-middle income countries (LMICs) as a cause area was also compiled by two other RTP researchers (their work can be found here: Cause Area - Improving access to pain relief in LMICs (Juan and Alex)). The authors focussed on approaches to reducing chronic primary and secondary pain in LMICs and explored three intervention strategies; first, advocacy for increased access to opioids in palliative care; second, supplying palliative care centers with opioids was proposed, with the aim to reduce opioid shortages where policies already exist; and third, outreach for use of migraine medications. Of the investigated interventions, the authors proposed looking further into using advocacy campaigns for opioid use during palliative care in LMICs. Their primary concerns relate to HLI’s cost-effectiveness calculations; particularly, the high household spillover rate of 53%, and uncertainties around the conversion rate between numeric pain rating scale (NPRS) and subjective well being (SWB) scales.
1.4 Intervention Scope
Despite back-of-the-envelope calculations supporting approaches to increase access to opioids in LMICs, a shallow dive into the matter revealed concerns around diversion of pharmaceutical opioids as a result of transport routes through Africa (United nations Office on Drugs and Crime, 2023). Several challenges and considerations for improving access to opioids include obtaining import and export permits, licensing physicians, nurses, and/or other healthcare workers to prescribe opioids, collaborating with a government body that regulates medications to ensure monitoring is possible, identifying qualified transport companies, ensuring tamper evident seals and a chain of signatures are used throughout the shipping process to track and authenticate all orders, monitoring sales patterns for upticks that may indicate diversion, among other considerations. Opiate-based pain medications are also subject to strict regulations due to their severe potential side effects. Since these regulations exist in high-income countries and appear sensible from a medical perspective (Joransen, 1990), we see few opportunities to bypass these regulations to improve access to opiates in low-income countries (LICs).
Although there is notable importance in overcoming barriers to accessing opioids for effective pain relief in PC patients, first, there is a seemingly greater need for establishing PC services in LMICs and enabling access to all forms of end-of-life support. This is is particularly apparent in Africa where PC is sparsely developed or equitable (Rhee et al, 2017). Therefore, we believe that creating conditions that allow for appropriate therapy with opiate-based pain medications in regions where opiates are medically approved and regulated at present, along with other evidence-based treatment approaches in life-limiting stages of disease, is a more promising approach to reducing suffering caused by substandard healthcare services.
2 Theory of change
The goal of this intervention is to reduce suffering and improve quality of life by increasing dignity and the ability to adapt to progressive diseases in regions where access to such relief is sparse or non-existent. This aim will be pursued through the effective alleviation of pain and other forms of severe health-related suffering (SHS). A new organization could aim to increase access to palliative care in countries with inadequate coverage.
2.1 Scope of the intervention
We propose improving access to PC through provision of medical advice, safe access to adequate pain management, as well as additional support if needed. The approach is to collaborate with existing hospitals and/or community health centers. The organization would attempt to identify gaps in the availability of PC and to address them systematically. To close these gaps, training would be provided to the local facility's hospital staff, and necessary materials and medications will be supplied. This is intended to enable palliative care for people in their home settings as well as ensure access to palliative support for those already hospitalized.
Explanation of color coding:
Green: We do not expect this uncertainty to be much of a burden
Orange: This might not be super easy to address and could be relevant regarding the expected success/ cost-benefit ratio of the intervention
Red: We expect this to be a high burden or uncertainty that could potentially kill the idea
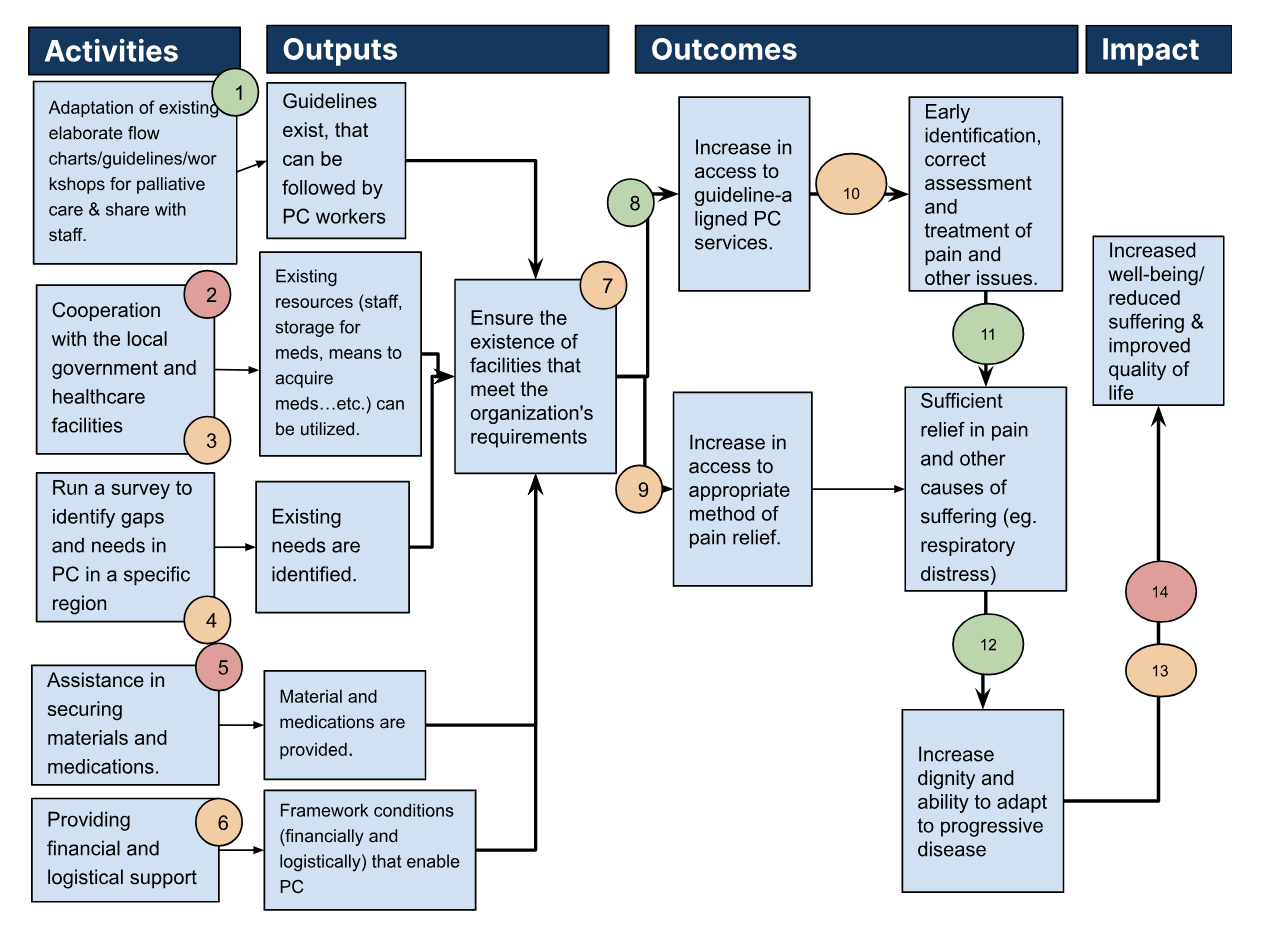
Activities
- Adapt existing flow charts/guidelines for palliative care that are easy to follow for field staff. Actor: organization's employees (can e.g. be done by the Founders = 2 P).
- Cooperation with the local government and healthcare facilities to utilize available resources for implementation/enhanced availability of palliative care.
- Run a survey to identify gaps and needs in PC in a specific region.
- Assistance in securing materials/medications, financial and logistical support.
Outputs
Intermediate Output:
- Guidelines that can be followed by PC workers
- Existing resources are being utilizes
- Existing needs are identified
- Material and medications are provided
- No financial or logistical burdens hinder PC center to exists
- Framework conditions (financially and logistically) are set up that enable PC
Final Output:
Ensure facilities that have trained staff, can provide access to medications and other necessary supplies, and can assist people with at-home care.
Outcomes
Intermediate Outcomes
- Increase in access to guideline-aligned PC due to providing guidelines and education of PC staff
- Increase in access to adequate pain medication due to ensuring general availability in PC centers and provision of home-care kits
Final Outcomes
- Early identification, correct assessment and treatment of pain and other issues.
- Sufficient relief in pain and other causes of suffering (eg. respiratory distress)
- Increase dignity, quality of life, and the ability to adapt to progressive disease
Impact
Increased well-being/ reduced suffering
2.3 Outlining assumptions and levels of uncertainty
- Assumption 1: Guidelines for palliative care exist and can be reframed to be easily followed by local healthcare staff
If we want to establish a sufficient treatment for severe health-related suffering, a guideline is necessary as it simplifies the treatment itself and allows for measurability of success in its implementation. We do not think this should be much of a burden, because guidelines for palliative care already exist with mention of international standards and it should be fairly easy to adapt them.
- Assumption 2: Collaboration with local levels of government is plausible.
To utilize available resources (e.g. existing healthcare centers/doctors/nurses/etc) as well as to source out some of the regulatory and organizational costs, it is essential to collaborate with local policymakers.
We see a large burden here, especially in countries with corrupt governance where funding for additional stocks of medication, health system monitoring, and other resources may not be prioritized. Tractability should therefore be well-represented in the GWFM and might outcompete other aspects.
Aside from quantitative proxies like the Fragile State Index’s components, it might also be worth looking at qualitative data such as whether other organizations have tried and failed to implement similar interventions.
- Assumption3: Collaboration with local healthcare facilities is plausible.
To utilize available resources (e.g. existing healthcare centers/doctors/nurses/etc) it is essential to collaborate with local healthcare facilities. Therefore things like their general willingness to cooperate and possible bottlenecks such as lack of capacity in terms of space and time, as well as personnel shortages, must be considered.
- Assumption 4: A survey is suitable for identifying gaps and needs in PC in the region the NGO is planning to operate.
To address a problem sufficiently it is necessary to identify the biggest needs, concrete bottlenecks, and gaps that need to be closed.
We assume that a survey can help identify these gaps and needs as well as serve as a tool for later evaluations.
- Assumption 5: Access to pain relief medication is relatively unimpeded.
The organization needs to ensure access to adequate pain medication. As we believe this might be one of the greatest burdens to overcome for a country without external support, this should be a top priority of the nonprofit organization. This is likely a major barrier to overcome in countries where opioids are illegal or disincentivized. That said, it could be controlled by choosing to operate in a country where legal or social barriers are minimal.
Means to mitigate drug stock-outs include: making sure there is more than one pharmaceutical supplier, requiring manufacturers to maintain an inventory of ingredients for critical drugs, having a third party (ie. government) keep a stock pile of critical drugs, and building redundancies in the drug supply. These tasks may be beyond the scope of a pilot intervention but could be worked towards through collaborations with government and health partners.
- Assumption 6: Nonprofits can assist local facilities in terms of financial and logistical support.
There might be some logistical or financial burdens a local facility would face when trying to implement a comparable intervention by itself, that are way easier to tackle for an organization working from abroad/having international contacts and reputation.
- Assumption 7: No additional considerations are required for the successful implementation of a well-equipped setting for palliative care.
To make the treatment accessible for people affected we would need to ensure facilities to have trained staff, can in practice provide access to medications and other necessary supplies, and can assist people with at-home care.
We expect there to be a broad variety of reasons why the named activities in our causal change do not necessarily lead to the establishment of well-equipped settings for palliative care in 100% of the cases (among others e.g. the density and quality of existing healthcare and the availability of medical personnel in the country where we want to operate).
This should be expressed in the CEA with a reasonable discount rate. We think it would be most accurate to incorporate different discounts for 'best case scenario', 'worst case', and 'median case' / 'best guess'.
- Assumption 8: Availability of trained staff does in fact increase access to guideline-aligned palliative care
The organization aims to ensure treatment according to the best available evidence on palliative care. The organization's approach to doing so is to provide guidelines, educate staff, and provide materials needed besides drug therapy/ in addition to drug therapy.
Thus it is not said that trained staff and the material accessibility of goods lead to accurate treatment in 100% of the cases.
This should be expressed in the CEA with a reasonable discount rate.
- Assumption 9: There are no unforeseen barriers to making the indication/ prescribing/ delivering/ administering pain medication
Ensure the access to adequate pain medication does not necessarily lead to patients in fact getting them. We expect there to be a broad variety of reasons why the mere availability of drugs does not necessarily lead to patients in fact getting and taking them in 100% of the cases. Among others we can think about the following barriers:
- (1) Indication -> prescription: People who are authorized to make the indication and prescribe the medication are needed (most likely doctors)
- (2) Stock -> patient: The drugs have to be delivered to the patients (stock to the patient)
- (3) Patient -> treatment: Patients need to be able/ willing to administer drugs
Opiophobia may reduce the efficacy of (1) and (3).
- Assumption 10: Increase in access to guideline-aligned PC and adequate pain medication leads to early identification and correct assessment of need as well as improved treatment
The measures addressed do not guarantee for achieving the intended effect of early identification, correct assessment, and treatment of pain and other issues in 100% of the cases.
This should be expressed in the CEA with a reasonable discount rate depending on how likely it is that meeting assumptions 8+ lead to early identification, correct assessment, and treatment of pain and other issues.
- Assumption 11: Early identification, correct assessment, and treatment of pain leads to sufficient relief of pain and other issues
If the need for adequate therapy is met we can be reasonably confident about it being beneficial for the people affected. Nonetheless, we should correct in some order of magnitude how much adequate therapy means in terms of relief in pain and other causes of suffering e.g. respiratory distress.
- Assumption 12: Relief in health-related suffering improves quality of life
If the need for adequate therapy is met we can be reasonably confident about it being beneficial for the people affected. Nonetheless, we should correct in some order of magnitude how much relief in pain and other causes of suffering e.g. respiratory distress means in terms of improving quality of life, and the ability to adapt to progressive disease. We suggest to use different conversion rates for best case, worst case and median case scenarios in CEA, to reflect the uncertainty here
- Assumption 13: Net change of Well-being of Intervention region is positive
We estimate that the net change of Well-being in the intervention region is positive. To estimate this we have to come up with an evidence-based conversion rate to convert pain/pain relief to WELLBYs and WELLBYS to DALYs
- Assumption 14: No unintended effects occur as a result of receiving palliative care from the organization.
Indicating the total effect of an intervention, potential negative indirect effects have to be taken into account.
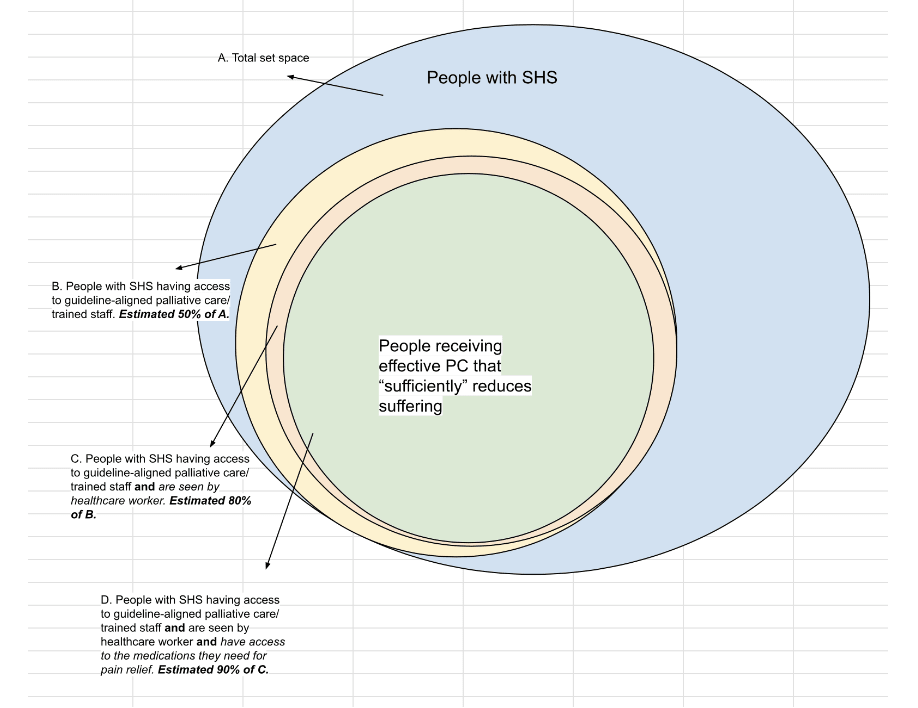
2.4 Approaches to Evaluation
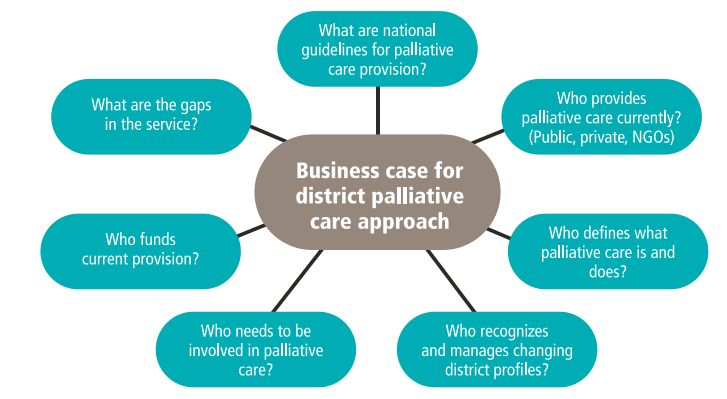
Before intervention begins, terminally-ill individuals and/or their caregivers should be surveyed in order to identify and assess needs. This could be accomplished by utilizing Hospice Africa Uganda’s Needs Assessment questionnaire (Kikule, 2003) or developing one alike. The figure below also highlights several key considerations that may help guide a needs assessment prior to formalizing intervention details.
From a monitoring & evaluation perspective it should be defined what indicators should be monitored by program staff to check if staff is indeed trained, access to medications and supplies have improved, and patients requiring PC do get them. Several means to assess quality of care exist in developed countries and may be referenced for this purpose but were not researched due to time limitations.
The intervention program should also come equipped with a means to measure its operational efficacy. This could benefit from further research.
Figure 2. Integrating palliative care into district health services - questions to consider (WHO Figure 10, p. 41)
3 Quality of evidence
3.1 Evidence that a charity can make change in this space
(This section’s content is taken from the links in section 6.2)
We did not find studies in the academic literature that evaluate the effectiveness of existing charitable organizations in this area; therefore, we rely on claims not sourced from the academic literature, but instead made by various organizations working in this space. Consequently, they should be interpreted with the awareness of potential biases. Collectively, the claims indicate that charities can indeed make change in this space on account of a noted increase in PC programming, augmentation of in-patient care with home visits, increased training of local healthcare personnel, and successful government collaborations. That said, we did not evaluate the cost-effectiveness or other measures of efficacy of these figures..
Hospice Africa
Hospice Africa claims the following impact figures:
- 37 countries now have palliative care due to their international programs work partnering with other organizations (only 3 countries when they started)
- 37,000 patients cared for at clinical centers, augmented by home visits and regularly scheduled mobile clinics at outreach sites
- 10,000 healthcare professionals have been trained via short courses and study programs
- Another achievement of Hospice Africa Uganda is in making available prescription of oral morphine by nurses and becoming the sole supplier of oral morphine in the country (p.37)
These figures suggest that it is feasible to provide palliative care by training local healthcare personnel. This report does not yet allow for statements concerning the cost-effectiveness of the measures.
Organization for the Prevention of Intense Suffering
The Organization for the Prevention of Intense Suffering (OPIS) claims the following impact:
- OPIS’s collaboration with Hospice Burkina (the palliative care association of Burkina Faso), with the goal of promoting access to morphine to all patients in need, resulted in a national conference on pain relief and palliative care officially supported by the Ministry of Health of Burkina Faso. This brought together “major stakeholders, including members of the government, doctors, other medical practitioners and pharmacists[…] to decide on concrete solutions to remove the obstacles” (e.g. lack of doctor training in prescribing morphine and overly strict regulations on morphine)
These figures suggest that it is feasible to cooperate with local governments and make political changes concerning regulations for provided aid. This report does not yet allow for statements concerning the cost-effectiveness of the measures.
Pallium India
Pallium India claims the following impact figures:
- Their 2021-22 annual report claims “3945 patients reached, 35,666 total patient contacts, 10,045 home visits, 1643 beneficiaries provided psychosocial support, 491 children provided education support, 300 physical aids & assistive devices provided, 180 beneficiaries provided food assistance”
- 4,800+ professionals trained both in-person and virtually, both in India (27 states and 6 UTs) and globally (Bhutan, Nepal, US, Australia, etc)
another page on the website of the organization names an even higher number (>6,000)
- Extensive track record of successful collaboration with governments (local, state and central levels) and the public, across policy development, integration of palliative care in the medical curriculum, and the establishment of 2 pain-free hospitals in partnership with “two major cancer hospitals in India”
These figures suggest that it is feasible to provide palliative care by training local healthcare personnel as well as to cooperate with local governments and make political changes concerning regulations for provided aid. Furthermore, these data demonstrate that an increased provision of palliative care does indeed result in more people being served.
Evidence on collaboration with local health networks
The success reports mentioned above indicate the feasibility of collaborating with local healthcare facilities. On the contrary a paper published by BMC Palliative care, part of nature communications, names low resources and competing priorities as main issues rather than knowledge about and access to palliative care as such.
The framework condition of a country's healthcare system isshould, therefore, be part of the GWFM since the intervention is fundamentally dependent on an existing healthcare infrastructure.
An expert Interview with Hospice Africa or success reports from other political organizations can be helpful to get a better sense of what are relevant burdens to face and what is plausible
3.2 Evidence that the change has the expected effects
There is high-quality evidence that pain relief medication reduces serious health-related suffering, but mixed evidence that most palliative care interventions reduce SHS. The following section elaborates on the latter.
In summary, we suggest that the uncertainty in PC interventions reducing SHS mainly relates to concerns associated with the measurability and feasibility of randomized studies in palliative care settings, rather than indicating a genuine absence of the effects of the interventions. Though there are challenges in conducting randomized control trials (RCTs) on palliative care patients (Visser et al, 2015), a more in-depth analysis of the evidence is needed to provide further validation for this hypothesis.
Evidence on effectiveness of varied PC interventions in developed countries
Aslakson et al. 2014 published a systematic review of 37 studies completed in the US and France evaluating 30 different interventions to better integrate palliative care and intensive care unit (ICU) care. The key takeaways are as follows:
- Evidence of effectiveness depended on outcome measured:
- Most interventions decreased hospital and ICU length of stay (LOS)
- All interventions (except two) had no effect on mortality
- Few interventions significantly affected family satisfaction
- No evidence of harm from any intervention
- Low evidence base quality made it hard to draw conclusions, due to
- Heterogeneity of interventions
- Heterogeneity of outcome measures
- Most studies being underpowered
- Most studies being subject to multiple biases
- The difficulty of assessing impact of interventions on family satisfaction (likely generalizes to other types of palliative care as well):
- High baseline family satisfaction (~70%) made many studies underpowered to detect statistically significant changes
- Patients and families might be invested in believing that they receive “good” care and reticent to criticize caregivers
Regarding this evidence, it seems necessary to note that it relates to palliative care in developed countries, not in low-income countries. Therefore, the effect cannot be directly extrapolated without discounting for generalisability. We are somewhat perplexed by the study's result that the interventions had no impact on mortality since palliative care is not intended to influence a patient’s prognosis. At most, it can be assumed that this conclusion signifies that there is no negative effect in terms of increased mortality, which would be a desirable outcome and align with the assertion that no adverse effects have been detected.
Interpreting the lack of improvement on family satisfaction, the authors of the study refer to a relatively high baseline satisfaction of families before the intervention. We assume that this could be different in LIC due to the absence of palliative care structures, potentially resulting in a larger spillover effect on family members than what may be demonstrated in the present study. However, a more detailed analysis in this regard is necessary before making substantiated assumptions, particularly when considering quantitative aspects.
Evidence on outcomes of various PC interventions
Ahluwalia et al. 2018 published an evidence synthesis of 139 systematic reviews of palliative care interventions, conducted with the goal of informing the fourth edition of the National Consensus Project Clinical Practice Guidelines for Quality Palliative Care. Despite substantial quantity of evidence, the quality of evidence remains low. Several factors affecting quality of evidence include:
- Few RCTs that allow strong evidence statements
- lack of precise effect estimates to support effectiveness of interventions
- inconsistency in study findings
- large variation in study designs
- What is still needed:
- more targeted efforts at strategically building the evidence base to conduct well-designed studies and provide high-quality support for specific palliative care interventions
- More attention towards opportunities to conduct RCTs (despite the challenges of doing so in some areas of palliative care)
- the use of other robust study designs examining key outcomes
The quality of evidence is summarized by intervention type (outcomes are from the supplemental file of the systematic review):
| Intervention type | Outcome(s) | Evidence quality |
| Home-based palliative care for frail homebound elderly patients (e.g. Martha et al 2016) | 1) more likely to die at home 2) Facilitates access to important services 3) allows patients to be cared for in their own home, as many express a preference for when asked about end-of-life care | High |
Music and art therapies (Bercovitz et al 2007)
Puetz et al 2013 suggest a few ways to improve methodological quality of research to study this intervention to improve evidence quality | Reducing anxiety and depression in patients with advanced illness | Moderate |
| Interdisciplinary team care | Positive outcomes related to - quality of life, - ACP, - death at home, - patient/family satisfaction with care | Moderate |
| Early/integrated palliative care for certain subpopulations such as patients with advanced cancer | - quality of life - physical symptoms - psychological health - mortality
Despite low-quality evidence, results are promising, which “underscore the need to continue to investigate this area across populations and settings, to build the evidence base for a practice that has significant face validity and growing empirical support” | Low
Very Low |
Grief and bereavement interventions
| “Reductions in distress and depressive symptomatology for family members identified at baseline as having the greatest amount of distress, depression, and social adjustment problems”
Hard to make conclusions about effectiveness due to “wide variation in how these services are resourced and delivered across the health system” | Low |
| Culturally sensitive palliative care | Reduce needless additional suffering from cultural insensitivities in care
This is a gap in the literature, since “acknowledging and incorporating sociocultural norms and practices in end-of-life care” is clearly important | Little to no evidence |
| Interventions focusing on unique needs of end of life patients | Reduce suffering related to end of life issues? “only two systematic reviews… and these were focused on pharmacological interventions” | Little to no evidence |
The rating named in the table above refers to the evidence quality of the systematic reviews for the intervention initially mentioned in the evidence synthesis article published by Ahluwalia et al. 2018. They tried to assess the quality of evidence using the Grading of Recommendations, Assessment, Development and Evaluations framework. They downgraded for study limitations (e.g., no randomized controlled trials contributing to the evidence), inconsistency in results across studies or lack of replication, imprecision (e.g., due to lack of reported effect estimates or imprecise estimates). They used the assessment of the systematic reviews evaluating the evidence base regarding indirectness, publication bias, or other criteria, where applicable.
Visser et al. 2015 echo the finding by Ahluwalia et al. 2018 regarding inadequate quality of evidence in the literature on palliative care effectiveness, and furthermore argue that
- palliative care lags behind other medical specialties in their development and use of evidence-based medicine (EBM) in clinical decision-making due to “the incompatibility of the fundamental assumptions and methodologies of EBM with the reality of their clinical contexts”, which makes it challenging to conduct high-quality RCTs, for example:
- The difficulty of recruiting a large-enough sample of consenting patients for studies to be adequately powered, due to a few recruitment barriers unique to the palliative care setting leading to a low percentage recruitment rate (e.g. Stone et al, 2013 reports only 8% of screened patients eventually enrolling)
- The difficulty of ensuring follow-up periods are complete enough for trials to be high-quality, due to high patient attrition rate mainly caused by high symptomatic deterioration (Hui et al, 2013)
- The difficulty of establishing clear links between interventions and outcomes, due to
- the challenge of controlling for the effects of interventions given the common practice of implementing packages of palliative treatments for multiple symptoms
- the challenge of achieving a balance between trial validity and trial generalizability in the heterogeneous palliative care population (Davidoff, 2011)
- the inappropriateness of traditional end points used in RCTs (e.g. death and disability) for the palliative population, and the difficulty of operationalizing the components of the goal of palliative care (improved quality of life), especially the psychological and spiritual aspects
- The ethical complexity of conducting RCTs in some palliative care settings (Leblanc et al, 2010)
- Suggestions to improve evidence quality for palliative care
- RCTs can be adequately powered by enlarging sample sizes via:
- increasing recruitment rates by designing studies to be “simple, non-invasive, and low-burden” with “well explained” experimental design (Stone et al, 2013)
- Using a collaborative research approach to pool resources (Abernethy et al, 2010)
- High quality non-RCT studies:
- mixed methods incorporating qualitative and quantitative analyses (cf. recent Medical Research Council guidelines)
- Observational studies of high quality, large sample size, and valid methodology (Benson & Hartz, 2000)
- RCTs can be adequately powered by enlarging sample sizes via:
In summary, it can be stated that various studies as well as active organizations in this field, describe positive effects concerning the enhanced quality of life due to palliative care. Thus the consistently described insufficient data regarding significant effects of palliative care measures raises concerns about the effectiveness of the intervention being evaluated here. Particularly, the fact that palliative care involves additional measures for alleviating suffering beyond mere pharmacological pain management fundamentally complicates drawing conclusions about the effect size of individual interventions. Nonetheless, reasons persist for adhering to the planned intervention. An aspect worth noting is that throughout all the studies, no averse effects have been reported.
3.3 Evidence on other key uncertainties
Assumption 1: Guidelines for palliative care exist and can be reframed to be easily followed by local healthcare staff
The following guidelines for palliative care were found with mention of international standards:
- Clinical Practice Guidelines for Quality Palliative Care
- See also: Planning and implementing palliative care services (p 14 f)
- WHO-recommended analgesic ladder
- APCA PalIiative Care Guidelines in Africa
Assumption 4: A survey is suitable for identifying gaps and needs in PC in the region the NGO is planning to operate
The WHO implemented a Needs Assessment using an interview created by Hospice Uganda for terminally ill persons or their caregivers. They also developed a network of PC professionals to advise the program planning, provide technical assistance, and help obtain resources.
We assume that a survey can help identify these gaps and needs as well as serve as a tool for later evaluations, thus other tools like focus groups, consultations, etc. could be equally valid.
Assumption 5: Access to pain relief medication is relatively unimpeded.
The World Health Organization includes opioids on the list of essential medications. Initially, this led us to assume that there should not be a significant regulatory obstacle to granting access to opioid-based pain medications. However, it appears that even an internationally operating organization must adhere to local regulations. Therefore, when considering the feasibility of the operation, a country that permits opioid therapy should be chosen. It should be noted that this could lead to countries with an even greater need in the evaluation being overlooked.
Several barriers to accessing medication may include:
- Costs: Due to the comparably low costs of painkillers (Sharma et al, 2020) we do not estimate costs to be a high burden for a nonprofit organization operating in this field.
- Regulations:
- Disincentives to prescribing opioids for pain relief exist in several countries; for example, in Ghana, prescription limits prevent opioids from being prescribed for more than 2 days and in 11 African countries, few local pharmacies are able to dispense opioids (Cleary et al, 2013).
- Although, it is legal to prescribe opioids in Zimbabwe, our proposed intervention region according to our Geographic Assessment, prescription rate is low (see 6.3 Operating in Zimbabwe), suggesting that disincentives may exist and should be further investigated. Disincentives may be reduced through health worker training and adequate guidelines.
3. Inventory
- We expect to leverage current pain medication stocks, although this assumes they are not in shortage. We did not do research on how to overcome this barrier.
4. Societal structure
- Collective attitudes towards medicines and end-of-life care
- Presence of multi-family or multi-generational households vs nuclear households.
- Could be easier to reach caregivers.
- Views on palliative care may be more easily influenced by other household members.
Assumption 11: Early identification, correct assessment, and treatment of pain leads to sufficient relief of pain and other issues
We are reasonably certain that opioid prescription reduces suffering and related issues. We are less certain that palliative care reduces suffering and related issues (section 4.2 elaborates on this). We therefore propose discounting the effect size of palliative care to account for mixed evidence quality.
Assumption 13: Net change of Well-being in Intervention region is positive
Though beyond the scope of this report, we suggest developing an evidence-backed conversion of SHS to WELLBYs.
Some considerations on this matter from HLI’s pain relief report:
- Conversion rates: 1 unit change (0-10 pain scale) → 0.12 units LS, or 1.09 units in negative affect and affective mental health
- Low estimate: having ‘extreme pain’ (versus ‘no pain’) in the EQ-5D is associated with losses of 0.5 (Graham et al., 2010), 0.7 (Mukuria & Brazier, 2013), or 1.3 life satisfaction points (Dolan & Metcalfe, 2012). Birkjær et al. (2020) found similar results with a different scale: going from ‘mild’ to ‘extreme’ pain (on a ‘mild, moderate, extreme’ scale) is associated with a loss of 1 life satisfaction point.
- For context: ‘extremely anxious or depressed’ ~ 3.6 LS points lost in Dolan and Metcalfe (2012)
- HLI says “consider going from ‘no pain’ to ‘extreme pain’ to be going from 0 to 10 on a pain scale, an 11-point change. Hence, we take the higher end of these estimates, 1.3 points, and divide by 11, to calculate that a one unit change on a 0-10 measure of pain will lead to a 0.12 unit decrease in life satisfaction.”
- High estimate: Psychology-based therapies for chronic pain reduce pain by 0.24 SDs and improve SWB (in negative affect and affective mental health measures combined) by 0.26 SDs -- so naively, “a 1-unit decrease in pain represents a 1.09-unit decrease in negative affect and affective mental health measures”, or ~9x the earlier estimate
- Why discrepant? HLI: “(1) perhaps psychotherapy for pain improves SWB through channels beyond reducing pain intensity (2) perhaps the regressions only measured life satisfaction whereas these RCT studies of psychology-based therapies measured negative affect and affective mental health”
- Low estimate: having ‘extreme pain’ (versus ‘no pain’) in the EQ-5D is associated with losses of 0.5 (Graham et al., 2010), 0.7 (Mukuria & Brazier, 2013), or 1.3 life satisfaction points (Dolan & Metcalfe, 2012). Birkjær et al. (2020) found similar results with a different scale: going from ‘mild’ to ‘extreme’ pain (on a ‘mild, moderate, extreme’ scale) is associated with a loss of 1 life satisfaction point.
- Difficulties in estimating conversion rates: it’s to model a dose-response relationship between pain and SWB, because
- It depends on what’s being asked & how respondents interpret it
- Pain can also affect SWB in indirect (instrumental) ways, e.g. pain and its causes “can cause disability or loss of function (which can incur social and economic consequences), preoccupy the mind, or lead to mental health problems”
- Pain affects others too: “by spreading through empathy, by needing others to help, or by lowering one’s social and economic participation”
These considerations seem somewhat confusing to us if not partially contradictory, and definitely not straightforward. Due to time constraints, we have not yet been able to come up with satisfactory considerations in this regard. An expert interview with HLI may help provide a better overview and understanding.
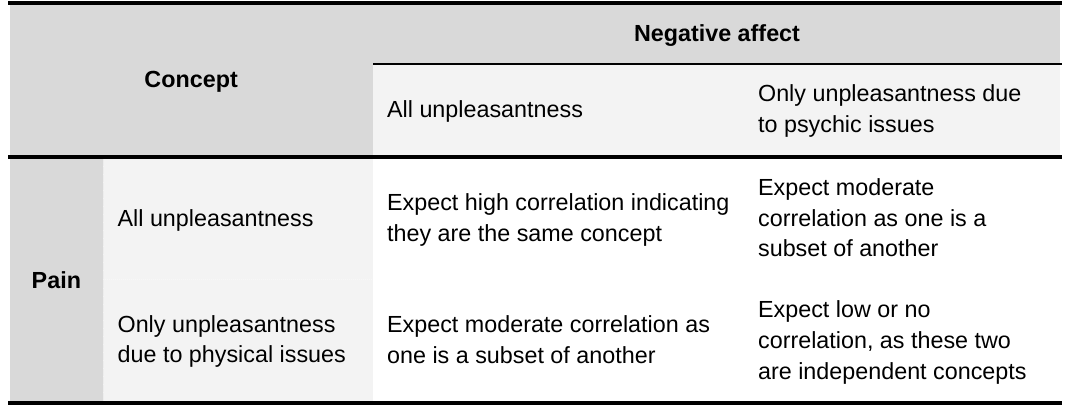
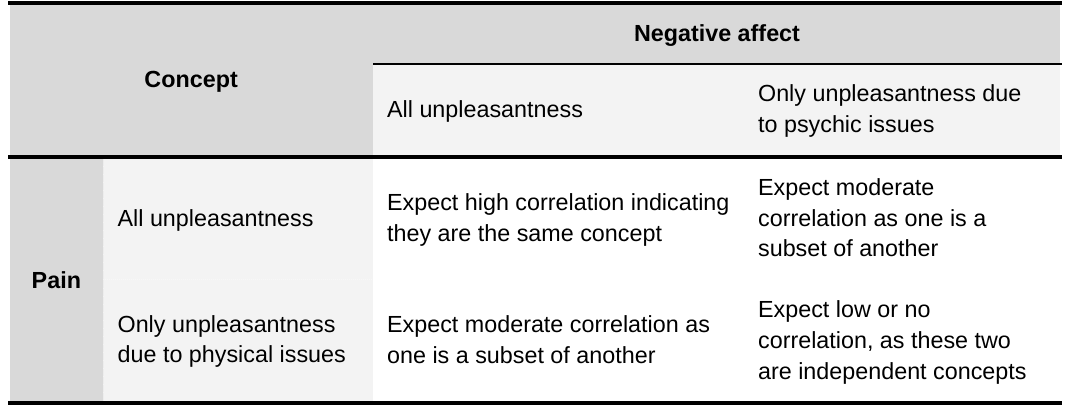
The table below from HLI’s pain relief report represents how they predict the strength of the dose-response relationship between pain and SWB from a search of literature:
Table 1. Happier Lives Institute’s prediction of dose-response between pain and subjective well-being.
Assumption 14: No unintended effects occur as a result of receiving palliative care from the organization.
Aslakson et al. 2014 didn't find any evidence of harm from any of the 30 different interventions they reviewed within a systematic review. Thus, as far as we can tell, they did not assess opioid-related palliative care, so opioid abuse may still be a concern.
5 Geographic assessment
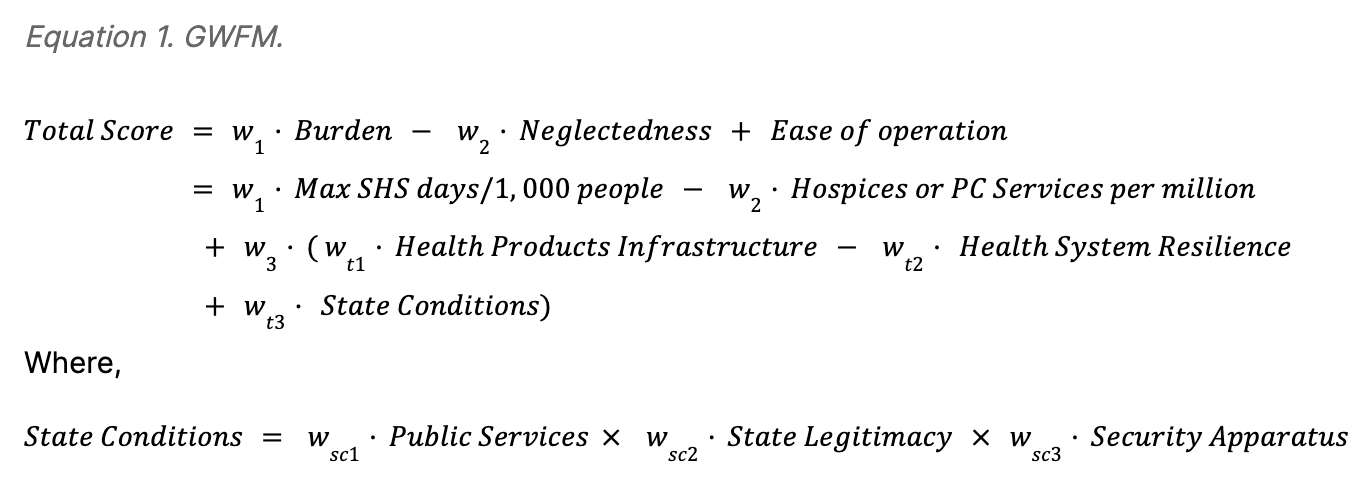
Globally, Sub-Saharan Africa (SSA) is referenced as one of the most under-developed and under-serviced region when it comes to awareness and provision of end-of-life care (Gysels et al., 2011). As such, it became the scope of the geographic assessment for this theory of change. We compiled inquiries pertinent to our Theory of Change, which could potentially influence both the feasibility of implementation and the ultimate impact of the intervention. We then tried to answer them as precisely as possible. First, we identified the area of greatest burden using the reported rate of serious health-related suffering, extracted from the International Association for Hospice and Palliative Care (IAHPC) database. Next, we considered conditions that would influence tractability of this intervention such as, current health care quality and infrastructure as well as conditions of the state. Thirdly, we considered where current intervention strategies are lacking. Finally, we conducted a formal geographic assessment using Equation 1. GWFM scoring to find the top candidate countries for starting a new nonprofit.
4.1 Geographic Assessment
4.1.1 Burden
The geographical evaluation of this intervention required different information sources. To assess the scale of the burden within SSA, we conducted a global analysis to ascertain countries with the most pressing need for palliative care. This entailed a quantitative assessment of the rate serious health-related suffering (SHS) per 1,000 population, extracted from the IAHPC database. The Lancet Commission defines SHS as any suffering that cannot be relieved without medical intervention and “when it compromises physical, social or emotional functioning” (Knaul et al, 2017). We think this is valid information to rely on, yet it is worth noting that data avaliable are from 2015.
4.1.2 Tractability
A tractable region for intervention was expected to be a locale that had some well-functioning pre-existing health care as well as suitable social environments that would allow for ease of program development and collaboration. This can be thought of as a proxy of “ease of operation”. To consider the quality of existing healthcare infrastructure and provisions, the World Health Organization’s Health Products Infrastructure (HPI) and (Health) System Resilience (HSR) Indicator were referenced. Both represent normalized indices; the former suggests the quality of physical infrastructure, such as presence of basic equipment and density of hospitals, healthcare centers, health posts, and hospital beds. Alternatively, the Health System Resilience indicator provides additional information on the following: awareness of essential services and quality of provisions; diversity in providing a broad range of services; functional mechanisms exist to ensure skills of staff and management are effective and updated; health care organizations are inter-operative and adaptable.
Social, or “state” conditions, were proxied through averaging three Fragile State Index indicators: (1) Public Services: the presence of basic state functions that serve the people; (2) State Legitimacy: representativeness and openness of government and its relationship with citizens; (3) Security Apparatus: internal and external security threats to a state and perceived trust of citizens in domestic security. All information referenced was used as input in the formal geographic assessment WFM to measure how much attention each issue is being paid.
4.1.3 Neglectedness
As an indicator of the neglectedness of palliative care within a country we incorporated information about the number of hospice or PC services per million into the geographic assessment. This includes data from the African Palliative Care Association (APCA) regarding the density of palliative care services per million inhabitants, according to population data from the World Bank.
This is in line with an evaluative survey conducted by the APCA in 2017 of ongoing efforts made to develop or enhance palliative care in specific geographic locales that offered insights on neglectedness. Here as well specifically, the density of hospices or palliative care services per million people was used to reveal proportionally under-serviced areas. For further investigation, it can be considered to incorporate a score capturing how much attention PC is getting, relative to other countries. For instance the percentage of a country’s Gross National Income spent on PC, or the status of Pain relief medication in a country’s essential medicines list.
4.1.4 Evaluation
We created a list of target countries using an average of subjective weights. One key factor was ease of operation (can also be thought of as tractability), which helped us rule out countries that were too challenging to work in. We put a fairly high weight on HPI and HSI aspects as we identified these as critical needs for success in our Theory of Change.
Assigning Weights
Weight values represent the average assignment by each author. Assignments were made as a proportion (value between 0 and 1) of the total score or, where multiple variables contribute to the development of one parameter, proportion of the resulting parameter. For example, State Conditions is composed of Public Services, State Legitimacy, and Security Apparatus; therefore, each of the latter was weighted as a proportion of the former.
| Parameter | Weight | Average Weight Value | Proportion of |
| Burden | w1 | 0.37 | Total Score |
| Neglectedness | w2 | 0.23 | Total Score |
| Ease of operation (Tractability) | w3 | 0.4 | Total Score |
| Health Products Infrastructure | wt1 | 0.37 | Tractability |
| Health System Resilience | wt2 | 0.3 | Tractability |
| State Conditions | wt3 | 0.33 | Tractability |
| Public Services | wsc1 | 0.33 | State Conditions |
| State Legitimacy | wsc2 | 0.38 | State Conditions |
| Security Apparatus | wsc3 | 0.29 | State Conditions |
We also set a limit on the scores related to people in the need of palliative care to a lower maximum. This was done to balance the impact of country size. Based on these criteria, we have identified the top 10 candidate countries for potential implementation:
Rank | Country | Total Score |
1 | Zimbabwe | 2.60909495 |
2 | Zambia | 1.287720251 |
3 | Sierra Leone | 1.225274269 |
4 | Central African Republic | 1.128487633 |
5 | Tanzania | 0.9475303288 |
6 | Ethiopia | 0.8741702325 |
7 | Eswatini (Swaziland) | 0.8066063304 |
8 | Gabon | 0.7952047614 |
9 | Kenya | 0.5185190137 |
10 | Cameroon | 0.4043611065 |
The remainder of the report will consider implementation of the proposed theory of change in Zimbabwe.
4.1.5 Data Quality
4.1.5.1 Exclusions
Countries with missing data in any of the indicators were removed as it was assumed that data were missing for several countries due to difficulty assessing the presence of physical and organizational healthcare infrastructure (See Appendix).
4.1.5.2 Vintage
Data used in the geographic assessment were published between 2015-2023. Rates of serious health-related suffering were the oldest data used in the assessment and also the most influential in evaluating need and top scoring regions. Updated data would likely result in different rankings.
4.1.5.3 Other considerations
The Quality of Death Index (2015) was not considered in this model as the SHS rates addressed the burden we defined but could be incorporated to assess need in future designs.
4.2 Where existing organizations work
The table below highlights key players recognized during research that focus on improving palliative care services in LMICs. This list was not heavily curated and is not intended to be comprehensive. A Global Directory of Palliative Care Institutions and Organizations is also made available from the International Association for Hospice and Palliative Care.
Organization | Description | Link |
| Hospice Africa Uganda | Hospice Africa set up a system with the Ugandan government for manufacturing and provision of liquid morphine (at-home remedies). | https://www.hospice-africa.org |
| Pallium India | NGO offering pain relief and palliative care as well as staff training in Trivandrum, Kerala. | https://palliumindia.org |
| Organization for the Prevention of Intense Suffering | They have collaborated with Hospice Burkina, the palliative care organization of Burkina Faso, to promote access to morphine and palliative care. | https://www.preventsuffering.org/ |
| Association for Palliative Care Centres (APCC) | The APCC currently has 91 members providing palliative care services throughout South Africa. Care is provided by an Interdisciplinary Team (IDT) that typically includes palliative care-trained Medical Doctors, Nurses, Social Workers, and Home-Based Carers. | https://apcc.org.za/ |
| African Palliative Care Association (APCA) | Pan-African organization to assess and assist in development of palliative care services. | https://www.africanpalliativecare.org/ |
| Organization for the Prevention of Intense Suffering (OPIS) | “Think-and-do” tank advocating for reduced suffering of sentient beings through governance. | https://www.preventsuffering.org/ |
| Diana, Princess of Wales Memorial Fund | Details are not mentioned on the organization’s web page but it is noted that the Princess of Wales Memorial Fund has previously implemented a Palliative Care Program in several African countries, including Zimbabwe. Whether it is still in operation is unclear. | https://en.wikipedia.org/wiki/Diana,_Princess_of_Wales_Memorial_Fund |
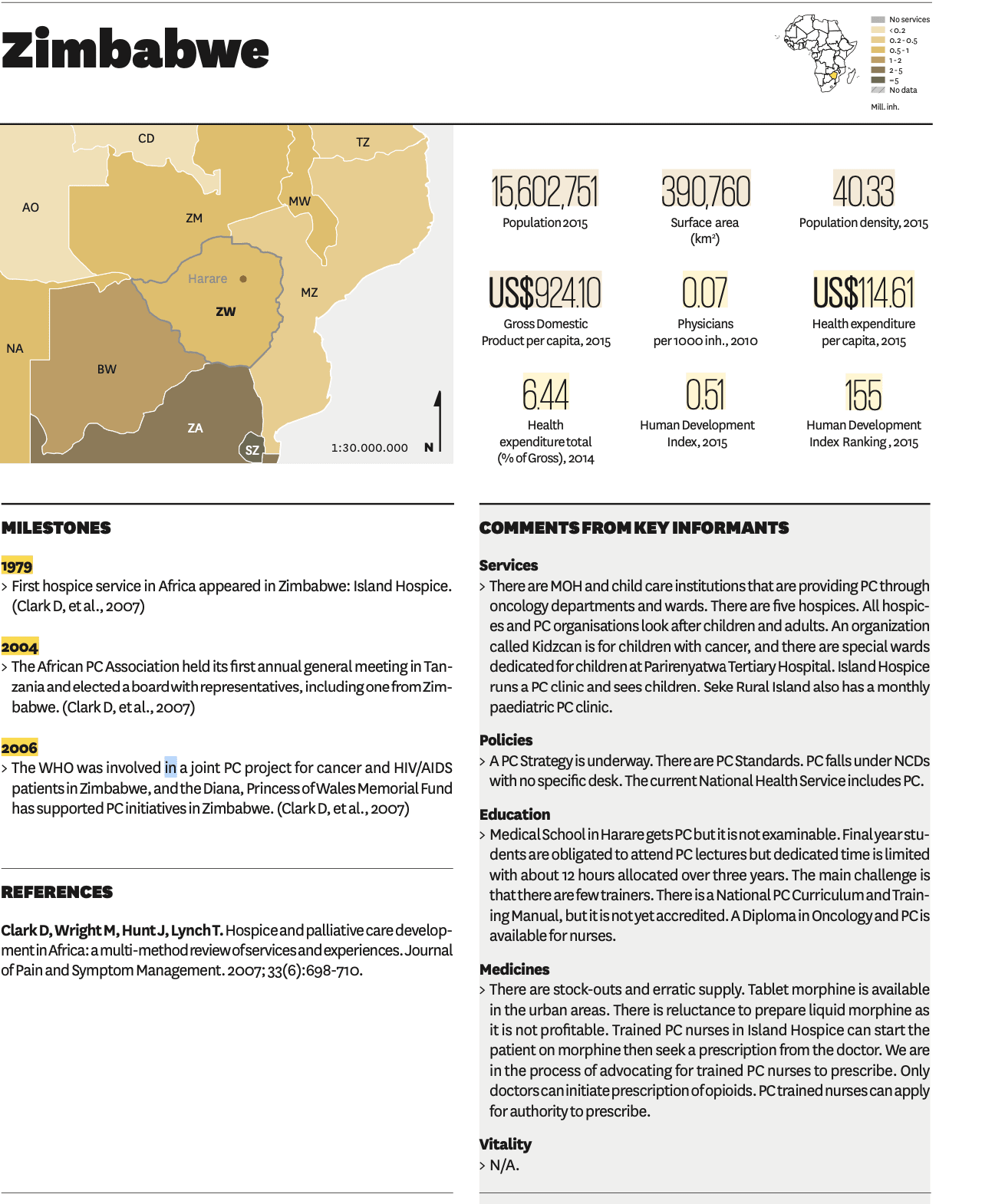
4.3 Operating in Zimbabwe
In 2017, the APCA released an Atlas of Palliative Care in Africa that describes the current landscape for healthcare and palliative care services for each country in Africa. Relevant statistics for Zimbabwe are highlighted in Figure 3. Notable current barriers to improving access to palliative care in Zimbabwe include:
- Ineligibility of non-specialised physicians to prescribe opiods. This may pose a challenge if task-shifting palliative care to community workers is chosen as part of the theory of change.
- Lack of staff training. This can ideally be resolved through the charity’s activities.
- National PC curriculum is not accredited for medical students. This can ideally be mitigated through the charity’s activities.
- Stock-outs and erratic supply of medications. Means to mitigate this barrier are proposed in Assumption 5 of the Theory of Change.
Figure 3. Country information on palliative care for Zimbabwe (APCA, 2017; pgs. 152-153).
5 Cost-effectiveness analysis (CEA)
#RTP23H4: [Improving Access to Palliative Care in LMICs] - Cost-effectiveness Estimate
Due to time constraints, this CEA is not fully fleshed out.
Year-based metrics like QALYs, DALYs, and WELLBYs may not be suitable for palliative patients (Smith et al, 2014), whose prognoses may be less than one year and whose measure of suffering can be reflected in days. Methodological challenges with converting measures of suffering to measures of subjective well-being are also noted. In line with the Lancet Commission’s estimation of palliative patient suffering, we thought it’d be more appropriate to evaluate cost-effectiveness by estimating the number of SHS days reduced through intervention.
Our cost-effectiveness calculation models a hypothetical 5-year program of free (worst-case) to low-cost (best-case) healthcare staff training in addition to free provision of at-home PC kits and services.
Based on our cost-effectiveness model, it was estimated that a new home-based palliative care program in Zimbabwe could reduce SHS by one day per patient for a cost between [$0.04, $1,350.40] USD with a geometric mean of $5.35. The primary concern of the calculation is the assumption that receiving palliative care reduces SHS days (Knaul et al, 2017). Note that this may not mean that suffering is eliminated but may propose that a patient receiving intervention is no longer categorized to be experiencing “serious” suffering.
We derived a potential conversion rate to disability-adjusted life years (DALYs) in the Appendix: A note on converting SHS days to WELLBYs.
5.1 Effects
The following considerations guided the estimation for effect of implementing new home-based PC programs:
5.2 Costs
To estimate costing, we decided on a top-down approach where funding determines the number of people receiving care (as opposed to a bottom-up approach that would estimate the cost of relieving all SHS individuals). In the above analysis, $100,000 was allocated annually to acquire and deliver pain medications and other palliative care products. Adjusting this parameter will affect estimations.
It’s assumed that philanthropic funding is expected to cover 100% of the organizational costs. Any increase in wages of local healthcare staff for the additional responsibilities is expected to be covered by government funding or negotiated through collaboration efforts. As such, staff wages are not included in the cost-effectiveness analysis. If the government is unable to fund staff wages, the potential cost-effectiveness of providing direct funding to governments or PC organizations may alternatively be investigated.
Figure 5. Parametric assumptions that influence cost-effectiveness estimates.
| Metric | Best Case | Worst Case | Remarks |
| Revenue from training program per health worker | Covered by philanthropic funding | Covered by healthcare staff receiving training | Worst case scenario is modeled after Hospice Uganda’s approach and generates revenue to support operations. |
| Count of people with SHS | - | Count of SHS stayed the same or declined over 8 years. 4,430 of SHS counts are attributed to malnutrition in Zimbabwe. No evidence supports a reduction in SHS counts since 2015 so it was assumed that the count remained the same as reported in 2015. | |
| Cost of pain medication (per patient per year) | Lancet Commission reports "$0.78 USD per capita per year" for the Essential Care Package in LMICs. | This is what HLI uses for their BOTEC on palliative care opioid supply. | Best case seems absurd and unreasonable. We do not trust this number. |
| Total SHS days reduced via pain medication |
Additional uncertainties that may impact estimates are noted in the CEA spreadsheet. It was also assumed that the start-up costs and annual organizational and overhead costs do not include other costs listed separately in the spreadsheet.
5.3 Discounts and Counterfactual Adjustments
Any deficiencies or barriers in delivering appropriate care was penalized in the bias. A lack of reportings on the coverage and operational reach by current organizations led to rough estimations for impact of this intervention. Other assumptions discounted by the CEA include biasing and generalizability.
6 Decision
At this stage of research, there are no crucial considerations in the theory of change that would discourage further advancement, evidence is generally in support of the theory of change and a rough estimation proposes this intervention to be cost-effective; however, quality of evidence could be reviewed. As such, we propose initiating a pilot project with monitoring and evaluation.
7 Implementation of a new idea
Start-up Activities
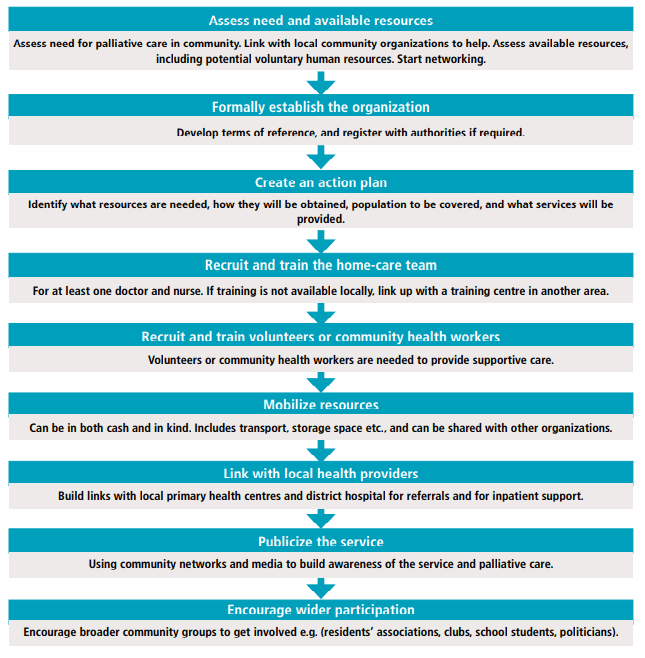
Due to time constraints, we were unable to elaborate on this section in detail. The flowchart below can provide an idea of what the WHO recommends. Additional considerations are highlighted in 3.4 Approaches to Evaluation. We recommend working closely with APCA who has developed a strategic plan to strengthen health care by incorporating PC from 2020 to 2030.
Figure 4. Steps for establishing a home-based palliative care service (WHO Figure 3, p. 20)
Developing At-Home Kits
Details from the Lancet’s Commission Panel 2: An Essential package of palliative care and pain relief health services may also guide development of at-home kits; particularly, which medicines and equipment to consider.
7.1 What does working on this idea look like?
Due to time constraints, we were unable to elaborate on this section in detail.
7.2 Key factors
This section summarizes our concerns (or lack thereof) about different aspects of a new charity putting this idea into practice.
Table 2: Implementation concerns
Factor | How concerning is this? |
Talent | Moderate Concern |
Access to information | Low Concern |
Access to relevant stakeholders | Moderate Concern |
Feedback loops | High Concern |
Funding | Moderate Concern |
Scale of the problem | High Concern |
Neglectedness | Low Concern |
Execution difficulty/Tractability | Low Concern |
Negative externalities | High Concern |
Positive externalities | Low Concern |
Talent
Given that the theory of change aims to leverage existing healthcare workers, collaborate with associations and local experts and levels of government, and incentivize employment of community workers by providing adequate training and pay, acquiring talent is not expected to be a significant barrier. Where appropriate, task-shifting may be applied to reduce the demand on specific health care practitioners (see Tables 3 and 10 of WHO’s guide for programme managers). Feasibility of these efforts may be better understood through an expert interview with a PC representative in Zimbabwe.
Access
Information
As the intervention is contingent upon this collaboration and many of the key actors presently operating in Zimbabwe and Africa are encouraging of improving PC services, it is not expected to be a barrier. Collaboration with local governments and health organizations is a key component to this operation that would involve cross-organizational sharing of information. APCA is likely the first point of contact and an organization with whom this intervention would work closely. APCA may offer local contacts in healthcare and government roles who would become additional collaborators.
Medicines
It is expected that the at-home PC kit would comprise medicines that are approved and accessible in Zimbabwe. If it is found that additional essential medicines should be included during collaboration with local healthcare providers, WHO (p. 55f) proposes the following considerations:
1. Approval/permission of the health ministry to register the medicine
2. Importation [of medication]
3. Contracting, pricing and estimating
4. Registration [of medication]
5. Import and export licensing
6. Storage, distribution and stocking
7. Education of prescribers
8. Community education
Relevant stakeholders
Currently it appears most likely that the key stakeholders and funders would be grants from general philanthropic donations. Therefore, it seems important to account for this in terms of a discount in the cost-effectiveness analysis and to consider additional potential stakeholders.
Feedback loops
Monitoring reach. Health workers can record their patient visits systematically either through the current capabilities of the local health system or by way of an extension to the system (ie. through a new means or standardization of reporting defined by the charity).
Monitoring prescriptions. It is expected that prescription-monitoring is a capacity of current health systems so would not pose additional challenges.
Measuring palliative care quality. It is also important to assess the quality of the palliative care provided. A number of outcome measures and indicators are available to measure the quality of palliative care. Standardized clinical tools should be used to measure symptom burden and functional ability regularly. (WHO, 2016. p. 66f)
See also: quality indicators mentioned in this publication and comparison of quality indicators detailed in this systematic review.
Measuring reduced suffering. We posit that reduced suffering may be measured through surveys of palliative patients and their caretakers; however, given the state of patients and variability in the experience of suffering, this may be challenging to draw conclusions from.
Funding
How much funding do they need in general over the course of their existence?
In order to provide continued care, funding would need to be persistent. Our cost-effectiveness estimate proposes that the first year of operation would cost about $100,000 plus fixed charity start-up costs. We estimate that this cost will be lower in the following years, as some starting as well as administrative costs would not longer have to be taken into account.
Please note that this is so far a very rough estimate and we are reasonably uncertain about the estimated numbers. Due to time constraints we did not include more detailed organizational costs and instead used CE’s estimates for fixed charity start-up costs.
Initially, we assume that all costs would be covered by the Charity and therefore funding corresponds fully to philanthropic donations. Staff training may also be covered by health care workers, as described in 7.2 Costs.he cost analysis by the WHO in the funding section of Planning and implementing palliative care services - A guide for programme managers (p. 37) leaves room for further exploration as to whether a distribution of costs to other funders, such as governments, may be promising in the long run.
Scale of the problem
In 2015, Zimbabwe had the highest rate of SHS in Africa of 81.55 per 1000 population as can be seen in the Global data platform to calculate SHS and Palliative Need. With Africa representing, on average, the youngest population globally, access to adequate palliative care may become paramount in relieving pain and suffering in the upcoming decades. In Zimbabwe, a continued population growth adds to the expected scale of burden in the future.
Tractability
From the Tractability conditions proposed through developing the GWFM, Zimbabwe appears to be fairly tractable. Potential limitations may include challenges in accommodating Zimbabwe’s 16 official languages; however, leveraging local staff should help to mitigate this concern. Securing relations with the government and current health organizations may also present challenges but is primarily expected to be welcomed (see the above section on Access to relevant stakeholders).
We tried to get a better sense about conditions contributing to tractability of Zimbabwe by looking at additional facts that might be relevant. That said, primary considerations should be given to the current PC and health care system in Zimbabwe outlined in 6.3 Operating in Zimbabwe, most notably, the regulations around morphine prescription.A lot of additional facts are listed on Wikipedia and would need to be fact-checked.
- 32 percent of Zimbabwe's inhabitants live in cities. Urban residents might have easier physical access to hospitals but staffing density and wait-times should be considered as well. 90 to 95 percent of the population are Christians, which may influence the holistic approach to providing PC.
- In 2018, Zimbabwe had 2.1 physicians practicing per 10,000 population (this is not a lot, but we lack comparisons with other african countries)
- Globally, Zimbabwe is among the countries most affected by HIV and AIDS (this might be the reason why it ranks that high in SHS)
- 16 official languages with equal rights (this might be challenging)
- Zimbabwe is named among the 20 countries that have improved the most in the last decade from 2010-20, according to the Fragile States Index, with the country consistently receiving one of the worst ratings in recent years. The Democracy Index has also shown cautious improvements since 2014, while remaining at a low level.
- With APCA’s strategic plan to incorporate PC in all levels of health care by 2023, we posit that the near future is a promising time for collaboration and implementation.
Externalities
Positive
It has been reported that improving access to palliative care reduces costs associated with unnecessary hospitalizations and medical interventions (Smith et al, 2014). This was not included in the CEA as it does not directly or measurably reduce suffering.
It is also possible that reduced suffering may have positive effects on households and community, as suggested by a large estimated spillover in Dupret et al. 2023.
Negative
Due to time constraints, comprehensive evaluation of potential adverse effects was not completed. Given that the organization will be dealing with substances susceptible to abuse, addiction, and severe side effects, we propose further investigation to estimate the extent and probability of such externalities arising.
We also expect the implementation of at-home palliative care to increase the burden on the healthcare system. This should be mitigated through task-shifting and/or training local community members.
Remaining uncertainties
The following uncertainties remain (note: this list is not intended to be comprehensive):
- How to estimate reduction of SHS days through deliverance of palliative care
- Whether staffing and medicinal resources will be available
- How readily accepted collaboration would be between current health organizations and government
- What the primary barriers will be in implementing at-home PC in Zimbabwe
9 Directing funding towards and existing entity
9.1 Governments
According to APCA’s Atlas of Palliative Care in Africa released in 2017, the majority of national governments in Africa reported having minimal funding for palliative care. This indicates that additional funding to support governmental development and endorsement of palliative care programs or subsidizing of universal medical expenses would probably be helpful for many African countries.
9.2 Current organizations
Among several smaller players, key established organizations that have aims in alignment with this proposed intervention strategy are listed below. For all, the impact of their initiatives on reducing suffering is not reported.
APCA
has also defined a set of palliative care guidelines, encourages governments to support affordable palliative care in public health services, provides training for community and professional care providers, and suggests research and monitoring and evaluation methods to ensure consistency in care is provided across the continent.
Effectiveness of operations: impact is not reported.
HOSPAZ
is a national private, voluntary association that has representatives in each district and aims to assess and support improvements of palliative care provision in Zimbabwe. The organization coordinates with palliative care providers to build capacity and advocacy.
Effectiveness of operations: from the HOSPAZ website, the mechanisms of action and impact in developing PCs is unclear. Webpages describing the program and palliative care are broken.
Island Hospice and Healthcare
was the first hospice in Africa, providing home-based palliative care in Zimbabwe since 1979. The organization follows the World Health Organization’s model for PC to offer clinical care, psychosocial support, and comprehensive capacity building for health professionals, spiritual leaders, communities, and alternative medicine providers (Khumalo & Maasdorp, 2016).
Effectiveness of operations: The Island Hospice and Healthcare website’s “Impact” webpage highlights the reach of their program services in terms of home and clinical visits, phone calls, and office consultations, among a few other metrics; however, an estimated reduction in pain and suffering is not reported. The organization claims to be audited by Deloitte & Touche annually. Audit reports may provide more insight into operations and impact but were not investigated for this report.
Hospice Africa
has been able to overcome barriers in access to medicine by providing at-home palliative care kits and lobbying for reduced restrictions in opioid-related policies (Jagwe & Merriman, 2007).
Effectiveness of operations: Hospice Africa established Palliative care in 37 countries that would otherwise most likely lack this kind of medical care. They managed to train 10,000 healthcare professionals via short courses and study programs.
Given the establishment of PC organizations in Zimbabwe, it may be helpful to support current organizations as they continue to mobilize access to and delivery of palliative care in African countries. Expert interviews to ascertain current roadblocks or organizational deficiencies in addition to conducting a cost-effective analysis estimating the counterfactual return of funding these organizations could provide a better understanding of the efficacy of current initiatives and whether a new organization in this space would bring about effective change.
9 Conclusion
After conducting a comprehensive examination of pain reduction in low-income countries (LIC) that focuses on the scale of the problem, potential barriers, conditions in individual states, and the cost-effectiveness of introducing at-home PC, we assess that the establishment of palliative care in Zimbabwe appears to hold potential, though this is subject to further validation. Specifically, we consider it a cost-effective measure for adequately addressing serious health-related suffering, including the provision of opioid-based pain medications. As such, we propose funding a pilot project with a monitoring & evaluation component to fill the evidence gap for effectiveness. As mentioned in section 8.2 Key factors, APCA’s aim to incorporate PC in all levels of health care by 2023 suggest that the near future is a promising time for collaboration and implementation of a home-based palliative care charity organization in Africa. Claims of success from existing organizations and the cause-area report from HLI regarding the order of magnitude of the problem addressed provide support for this suggestion.
10 Additional considerations
With more time, the following concepts would be investigated:
- In contradiction to the proposed strategy for ameliorating suffering in LMICs, Lancet Commission attributes over half of the burden suffering in LMICs to preventable deaths (Knaul et al, 2017), which raises the question whether it would be more effective to introduce an intervention that focuses on preventing such outcomes. At the time of writing, we have not explored this alternative.
- In depth research on navigating regulatory barriers for accessing opioid medications in SSA.
- Studies and reviews on quality of palliative care.
- Differences in burden, needs, and delivery of palliative care to children versus adults.
References
- Abernethy, A.P., Aziz, N.M., Basch, E., Bull, J., Cleeland, C.S., Currow, D.C., Fairclough, D., Hanson, L., Hauser, J., Ko, D., Lloyd, L., Morrison, R.S., Otis-Green, S., Pantilat, S., Portenoy, R.K., Ritchie, C., Rocker, G., Wheeler, J.L., Zafar, S.Y., Kutner, J.S. (2010). "A strategy to advance the evidence base in palliative medicine: formation of a palliative care research cooperative group." J Palliat Med, 13(12), 1407–1413. https://doi.org/10.1089/jpm.2010.0261
- Aslakson, R., Cheng, J., Vollenweider, D., Galusca, D., Smith, T.J., Pronovost, P.J. (2014). "Evidence-based palliative care in the intensive care unit: a systematic review of interventions." J Palliat Med, 17(2), 219–235. https://doi.org/10.1089/jpm.2013.0409
- Benson, K., & Hartz, A. (2000). "A Comparison of Observational Studies and Randomized, Controlled Trials." N Engl J Med, 342, 1878–1886. DOI: 10.1056/NEJM200006223422506
- Clark, D., Wright, M., Hunt, J., & Lynch, T. (2007). "Hospice and Palliative Care Development in Africa: A Multi-Method Review of Services and Experiences." https://doi.org/10.1016/j.jpainsymman.2006.09.033
- Cleary, J., Powell, R. A., Munene, G., Mwangi-Powell, F. N., Luyirika, E., Kiyange, F., … Cherny, N. I. (2013). "Formulary availability and regulatory barriers to accessibility of opioids for cancer pain in Africa: a report from the Global Opioid Policy Initiative (GOPI)." Annals of Oncology, 24(suppl 11), xi14–xi23. doi:10.1093/annonc/mdt499
- Connor, S., et al. (2020). "Global Atlas of Palliative Care: 2nd Edition". ISBN: 978-0-9928277-2-4. https://cdn.who.int/media/docs/default-source/integrated-health-services-(ihs)/csy/palliative-care/whpca_global_atlas_p5_digital_final.pdf?sfvrsn=1b54423a_3.
- Davidoff, F. (2011). "Heterogeneity: we can't live with it, and we can't live without it." BMJ Qual Saf, 20 Suppl 1(Suppl_1), i11–i12. doi: 10.1136/bmjqs.2010.046094
- Dupret, S., McGuire, J., & Plant, M. (2023). "Pain relief: a shallow cause exploration." https://www.happierlivesinstitute.org/wp-content/uploads/2023/02/Pain-relief_-a-shallow-cause-exploration-MASTER-1.pdf
- Gysels, M., Pell, C., Straus, L., Pool, R. (2011). "End of life care in sub-Saharan Africa: a systematic review of the qualitative literature." BMC Palliat Care, 10, 6. doi: 10.1186/1472-684X-10-6
- Hui, D., Glitza, I., Chisholm, G., Yennu, S., Bruera, E. (2013). "Attrition rates, reasons, and predictive factors in supportive care and palliative oncology clinical trials." Cancer, 119(5), 1098–1105. doi: 10.1002/cncr.27854
- International Association of Hospice and Palliative Care. (2015). "Global Access to Palliative Care and Pain Relief." https://hospicecare.com/what-we-do/projects/global-data-platform-to-calculate-shs-and-palliative-care-need/database/.
- Jagwe, J. & Merriman, A. (2007). "Uganda: Delivering Analgesia in Rural Africa: Opioid Availability and Nurse Prescribing." https://doi.org/10.1016/j.jpainsymman.2007.02.014
- Joranson, D.E. (1990). "Federal and state regulation of opioids." J Pain Symptom Manage, 5(1 Suppl), S12–S23. PMID: 1969888.
- Khumalo, T. & Maasdorp, V. (2016). "The Island Hospice model of palliative care." Ecancermedicalscience, 10, 654. doi: 10.3332/ecancer.2016.654
- Kikule, E. (2003). "A good death in Uganda: survey of needs for palliative care for terminally ill people in urban areas."
- Knaul et al. (2017). "Alleviating the access abyss in palliative care and pain relief—an imperative of universal health coverage: the Lancet Commission report." http://dx.doi.org/10.1016/S0140-6736(17)32513-8
- Rhee, J., Luyirika, E., Namisango, E., Powell, R., Garralda, E., Pons, J., de Lima, L., & Centeno, C. (2017). "APCA Atlas of Palliative Care in Africa." IAHPC Press.
- Ahluwalia, S., Chen, C., Raaen, L., Motala, A., Walling, A.M., Chamberlin, M., O'Hanlon, C., Larkin, J., Lorenz, K., Akinniranye, O., Hempel, S. (2018). "A Systematic Review in Support of the National Consensus Project Clinical Practice Guidelines for Quality Palliative Care, Fourth Edition." Journal of Pain and Symptom Management, 56(6), 831–870. https://doi.org/10.1016/j.jpainsymman.2018.09.008
- Sharma, S., Donaldson, C., Plant M. (2020). "Global Priority: Pain." Happier Lives Institute. https://www.happierlivesinstitute.org/wp-content/uploads/2022/04/Global-priority_pain.pdf
- Smith, S., Brick, A., O'Hara, S., Normand, C. (2014). "Evidence on the cost and cost-effectiveness of palliative care: a literature review." Palliate Med, 28(2), 130–150. doi: 10.1177/0269216313493466
- Stone, P.C., Gwilliam, B., Keeley, V., Todd, C., Kelly, L.C., Barclay, S. (2013). "Factors affecting recruitment to an observational multicentre palliative care study." BMJ Support Palliat Care, 3(3), 318–323. doi: 10.1136/bmjspcare-2012-000396
- LeBlanc, T., Wheeler, J.L., & Abernethy, A.P. (2010). "Research in End-of-Life Settings: An Ethical Inquiry." Journal of Pain & Palliative Care Pharmacotherapy, 24(3), 244–250. DOI: 10.3109/15360288.2010.493579
- United Nations Office on Drugs and Crime. (2023). "World Drug Report: Special Points of Interest." https://www.unodc.org/unodc/en/data-and-analysis/world-drug-report-2023.html
- Visser, C., Hadley, G., Wee, B. (2015). "Reality of evidence-based practice in palliative care." Cancer Biol Med, 12(3), 193–200. doi: 10.7497/j.issn.2095-3941.2015.0041
- World Health Organisation. (2018). "The state of health in the WHO African Region: an analysis of the status of health, health services and health systems in the context of the Sustainable Development Goals." Brazzaville: WHO Regional Office for Africa; Licence: CC BY-NC-SA 3.0 IGO.
- World Health Organization. (2016). "Planning and implementing palliative care services: a guide for programme managers." https://iris.who.int/bitstream/handle/10665/250584/9789241565417-eng.pdf